Pressure Injury Toolkit For Spinal Cord Injury and Spina Bifida
Beyond the wound - Bringing best practice to the bedside

Causative and contributing factors - Management
Manage SCI and SB -specific factors and other medical conditions
Address SCI and SB -specific factors, such as the following:
- Level and extent of SCI impairment
- Previous Pressure Injury
- Ageing
- Autonomic Dysreflexia
- Bladder and bowel incontinence
- Cardiometabolic Disease
- Heterotopic ossification or fracture
- Poor Nutrition
- Psychological / Mental Health Disorder
- Shoulder / upper limb pain and injury
- Spasticity and contracture
Comprehensive management of SCI and SB-specific and other medical conditions
Comprehensive management of SCI and SB -specific and other medical conditions
SCI and SB-specific factors and other medical conditions
| FACTOR | INFORMATION |
|---|---|
Level and extent of SCI impairment | Monitor routinely for signs of neurological loss in relation to original level and severity of impairment that may indicate an extension of cord damage. Changes that are detected at an early stage are more likely to be successfully managed (for example, by neurosurgery for insertion of a shunt to drain a syrinx). |
Previous Pressure Injury | Optimise overall health and wellbeing and monitor a high risk individual more frequently, with regular scheduled screening and assessment of skin and general health. |
Time since injury | Ensure that the individual is aware of the ongoing and changing risks to skin integrity over time, and use proactive management strategies to mitigate risks, such as maintaining muscle mass, reducing upper limb overuse and treating chronic conditions, such as obstructive sleep apnoea (OSA). Provide regular education, monitoring and scheduled health maintenance reviews as part of standard practice. |
Acute illness | For individuals with SCI or SB who are most at risk of secondary health conditions or experience frequent hospitalisations, it is useful to develop an Individualised Care Plan (ICP) detailing what care is needed and how it is to be provided. The ICP is usually developed in consultation with the spinal medical, nursing and allied health team. It documents person’s relevant clinical information, specific needs, care routines, level of assistance, equipment requirements and strategies to reduce risk of bladder, bowel, skin and other health complications during an unplanned admission for acute illness. |
Ageing | Some age-related changes that can increase PI risk may be modifiable in the person ageing with a SCI, such as nutrition, muscle mass through activity and strength training and monitoring of mood and support. Being proactive to address these known risk factors with regular scheduled spinal multidisciplinary team reviews, assessment of mobility equipment, personal care needs and domestic support may reduce risk of PI. |
Autonomic Dysreflexia | The presence of a wound and/or examination of a wound may provoke an episode of autonomic dysreflexia (AD). It is essential that both patients and staff know the signs and symptoms of AD, the risk factors, likely causes and what to do in the case of an emergency. Consider suitable prophylaxis or adequate analgesia prior to wound dressing. For further information, refer to the AD treatment algorithm. |
Bladder and bowel dysfunction | Regularly review management strategies to reduce contributing factors associated with poor bladder or bowel routines, including reducing the duration of bowel care, recommending appropriate equipment, ensuring the required assistance is available and incontinence is managed. A pro-active assessment of an individual’s bladder and bowel program may reduce skin trauma and improve wound healing. Short-term strategies may be required, such as insertion of an indwelling catheter to facilitate care on bed rest or temporary colostomy to avoid wound soiling. |
Cardiometabolic Disease (CMD), Peripheral Artery Disease (PAD), Diabetes | For those at risk of CMD, specific advice and management about weight management and nutrition, physical activity and exercise, lifestyle and medications to control risks associated with obesity, insulin resistance, dyslipidemia (including individual risks of low high-density lipoprotein cholesterol (HDL-C) and elevated Triglycerides (TG), and hypertension for persons with SCI should follow best-practice guidelines12. Refer to vascular specialist for investigation of PAD and referral to vascular surgeon is recommended. |
Cognitive Impairment | Provide behaviour management support with more structured environment and memory aids, rationalise medications, institute a regular routine of skin inspection with suitable equipment. Review drug and alcohol intake (including prescribed, over-the-counter and any elicit medications), which could be affecting cognitive functioning. In the older person, in particular, reassess the need for anticholinergics, narcotics, sedatives and benzodiazepines. |
Heterotopic Ossification
| Heterotopic ossification (HO) may increase the risk of developing a PI; for example, due to limitation of range of motion or effects on posture and seating position. Once HO has developed to the extent that it contributes to significant secondary health complications, such as skin breakdown, and/or severe functional interference, surgical intervention is most likely the only option and requires careful assessment and planning regarding timing and further post-operative management. |
Leg fracture | Application of additional padding with use of bivalve or removable casts to allow skin inspection is recommended to prevent PI developing over the skin of an immobilised lower limb. Consultation with specialist spinal services is strongly recommended where immobilization is required. A period of hospitalization, specialist seating assessment, hire of pressure relieving equipment (e.g. cushion or mattress) and an increase of personal care hours are all likely to be required. |
Pain | Ensure that the individual has an appropriate pain management program, which may include pharmacological and non-pharmacological approaches. See the ACI Chronic Pain website for more information. |
Poor Nutrition
| Adequate energy and protein intake is necessary to sustain optimal metabolic functioning and support healing. Management to prevent/improve malnutrition includes restoration of a well-balanced diet with ample caloric intake and adequate micronutrient replacement. See Optimise nutrition and address malnutrition for more information. |
Psychological / Mental Health Disorder | Refer to sections in toolkit on Depression, Substance Use, and Exacerbation of Pre-existing Mental Illness/Disorder. |
Respiratory complications | It is essential that the individual is given a breathing exercise program during any period of bed rest. |
Shoulder / upper limb pain and injury | Consider referral to an occupational therapist or physiotherapist to assess the extent to which upper limb impairment impacts upon mobility and transfers. An exercise program or equipment review may be required. |
Spasticity and contracture | Severe, uncontrollable muscle spasms may increase the risk of developing a PI through friction on skin or functional interference, such as making transfers more difficult. Treatment may be with oral, intramuscular or even intrathecal medications, depending on whether localised or generalised. Surgical procedures to lengthen/divide tendons or treat joint contractures may sometimes be required. |
Smoking | All efforts should be made to encourage smoking cessation and strategies such as nicotine patches, and counselling support should be offered. |
Optimise nutrition and address malnutrition
Numerous strategies may be necessary to manage an individual’s nutrition status. Referral to a dietitian is recommended:
- Early nutritional support
- Strategies to facilitate access to nutrition
- Calculation of SCI and SB-specific calorie, protein and fluid intake
- Consideration of Arginine, supplements and enteral feeding in accordance with precautions and contraindications.
Comprehensive management of nutrition and addressing malnutrition
Comprehensive management of nutrition and addressing malnutrition
- Numerous strategies may be necessary to manage an individual’s nutrition status.
- Enhance meals and snacks by incorporating liquid or powder supplements and initiating vitamin and mineral.
- Supplementation and providing enteral or parenteral nutritional support may be required.
Nutritional intake and support:
- Implement early nutritional support measures if dietary intake is inadequate or if an individual is nutritionally compromised.20
Access to nutrition:
- Consider the individual’s ability to self feed or the amount and type of assistance needed for eating and drinking. People at greatest risk of malnutrition and dehydration are those who are dependent on others for food and fluid.
Calorie, protein and fluid intake :
- For adults with SCI calorie, protein and fluid requirements are (for Stage 2, 3, 4 pressure injuries)51:
Paraplegia 25.9 ± 1.2 kcal/kg/day 1.25 – 1.5g/kg/day protein
Tetraplegia 24.3 ± 1.1 kcal/kg/day 1.25 – 1.5g/kg/day protein
Fluid: 1ml/kcal/day + 500ml
Arginine:
Supplements:
- Consider supplementing vitamins and minerals in people with known deficiencies to improve PI healing. Use clinical judgement and the results of a thorough nutritional assessment to determine the need for nutrient supplementation in the absence of definitive tests for deficiencies.20
- Avoid Vitamin E supplementation as it may delay healing20
- Avoid high levels of zinc2
- Identify all conditions that may have precautions or contraindications for supplementation, such as renal insufficiency, before implementing micronutrient, protein or fluid supplementation.20
Enteral nutrition:
- Provide enteral nutrition to support PI healing, if indicated, when the gastro-intestinal tract is intact but dietary intake is inadequate and/or barriers to oral intake exist. Provide total parenteral nutrition, if indicated, to individuals with PI and GI disease or dysfunction.20
Manage mechanical factors
Pressure, friction, shear and microclimate over the 24 hour period.
Mechanical factors that are not the cause can still impair healing by reducing tissue tolerance or increasing pressure.
Spinal cord injury-specific factors amplify risk
Spinal cord injury-specific factors amplify risk
SCI and SB-specific factors amplify risk
SCI and SB-specific risk factors increase exposure to extra pressure or reduce the skin’s ability to tolerate pressure.
Pressure
As a result of a SCI or SB, people are more susceptible to the effects of direct pressure due to: (i) impaired or absent protective sensation below the level of injury (e.g. loss of pain, temperature, pressure and light touch sensation), (ii) muscle paralysis which limits mobility, ability to transfer and re-distribute body weight, often requiring a wheelchair or assistive device and, as a result, (iii) significant limitations to functional activity.
Extrinsic Factors
Extrinsic factors reducing tissue tolerance for people with SCI or SB include: (i) increased moisture from hyperhidrosis, long periods of sitting or from possible bladder or bowel incontinence; (ii) friction from reduced clearance during transfers, poorly fitting equipment or clothing; and (iii) shear from sliding down the bed, reduced lift or clearance when re-positioning, muscle spasticity or sliding forwards in a poorly set-up wheelchair.
- Moisture
- Friction
- Shear
Intrinsic Factors
Intrinsic factors reducing tissue tolerance for people with SCI or SB include: (i) impaired circulation from autonomic nervous system and cardiovascular changes, and, decreased muscle pump reducing venous return and the delivery of oxygen to the muscles; (ii) use of medications that reduce alertness; (iii) increased risk of malnutrition; (iv) high prevalence of comorbidities and other chronic diseases; and (v) secondary conditions such as shoulder pain reducing the ability to lift and transfer body weight during daily mobility and self-care activities.
- Oxygen delivery
- Medications
- Demographics
- Nutrition
- Chronic illness
- Pain
- Skin
- Temperature
Braden & Bergstrom (1987)
The 24 Hour Approach
It is critical to evaluate sources of excessive or prolonged pressure, friction, and shear, and problems with local skin temperature and moisture to make suitable alterations in equipment and daily activities to maximise function while minimising trauma to the affected area.20
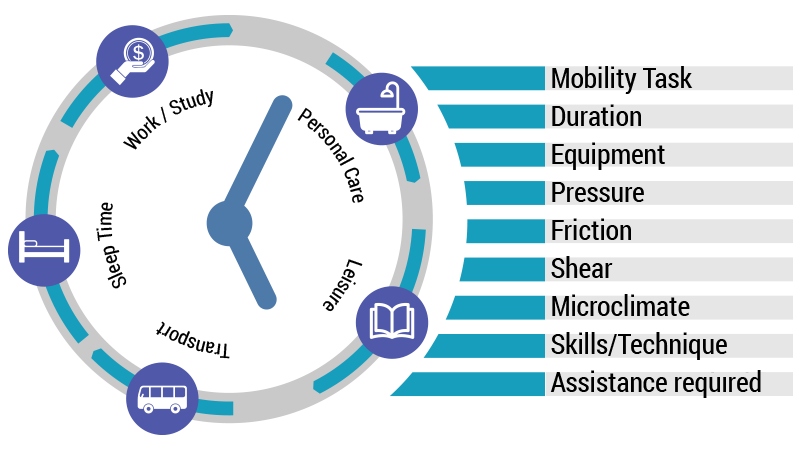
Strategies to address mechanical factors include:
Minimise sitting time and consider ‘bed rest’
Minimise sitting time and consider ‘bed rest’
If the red mark, graze, blister, ulcer or injury on the skin is located over a bony prominence against the sitting surface, remove pressure immediately to prevent progression of the wound. This will often require bed rest, lying off the affected area, until the cause and contributing factors can be investigated and addressed.
Avoid prolonged bed rest and re-evaluate the pressure management plan with an interdisciplinary team.20
Avoid prolonged bed rest by:
Acting quickly
- Remove pressure immediately
- Have a plan in place that supports the person to spend increased time in bed. This will include maximising the amount of paid and unpaid assistance received.
Identifying all possible contributing factors20,11,32
- Address each of them with the person, carer and interdisciplinary team.
- Factors that are not necessarily the cause of the PI can still impair wound healing by reducing tissue tolerance or increasing pressure.
Optimising all support surfaces20,11,32
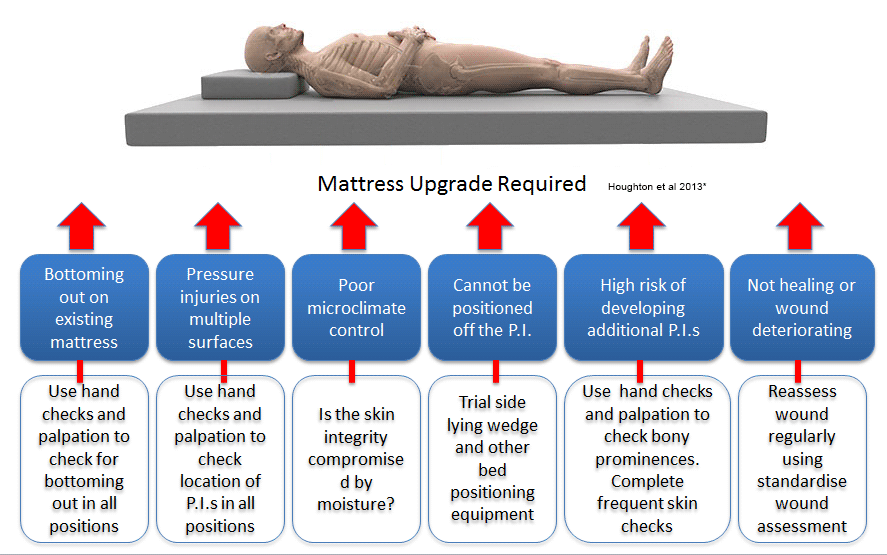
- Upgrade the mattress (if required) to prevent additional skin breakdown
- Arrange a seating assessment as soon as possible
Once the seating system has been:- optimised to reduce pressure loading to the affected area,
- effective pressure relieving or weight shift strategies determined and
- short increments of sitting have been trialled with close monitoring of the skin,
the interdisciplinary team (including the tertiary team) and the client can determine the feasibility of sitting, sitting duration and a sitting schedule.
For example, depending on risk factors, resources and complications of bed rest experienced, for some clients this might include sitting to attend appointments only while for other clients, it might include sitting for 2 hours each day.
- Avoid or limit the frequency and duration of commode / toilet / shower chair usage and optimise pressure management
Implementing a range of pressure management strategies 20,11,32
Using a 24 hour approach, implement a range of pressure management strategies including:
- Safe positions in bed and a repositioning schedule
- Slide sheets to reduce friction and shear when repositioning
- Transfers that do not cause further trauma to the skin (consider an electric bed to adjust bed height for easier transfers; consider hoist to eliminate friction and shear when lifting to transfer).
- Maximum care taken to put a hoist sling in place and to remove it.
Prevent complications of bed rest20,11,32:
Show table of complications and preventative strategies
Complication | Prevention Strategy |
|---|---|
Deep Venous Thrombosis (DVT) | People with SCI and SB are at increased risk of developing DVT due to immobility, paralysis, cardiovascular and autonomic system compromise. In addition, an individual with a PI and minimal sitting time or bed rest is at increased risk of developing a DVT. Refer to General Practitioner or other treating medical specialist for prescription of anticoagulant medications and advice if the individual is to be immobilised or on bed-rest for a period of time, in accordance with current clinical practice guidelines. |
Pulmonary Embolism (PE) | Consider early referral to GP for anticoagulants and monitor for the following signs: Chest pain on deep inspiration, shortness of breath, possible blood in sputum. Investigate with spiral CT or V/Q scan.
|
Pneumonia | Refer to physiotherapist for an individualised deep breathing exercise program that aims to clear and inflate lungs regularly and is based on how much difficultly a person has clearing secretions. Secretions need to be mobilised daily through quad coughing, mechanical insufflator –exsufflator or glossopharyngeal breathing. Increase preventative strategies if signs of a cold, bronchitis or upper respiratory tract infection develop. Burns, S. (2004) SCI Forum Reports: Common Respiratory Problems in SCI: What You Need to Know (washington.edu).
|
Secondary pressure injuries |
|
Dehydration and malnutrition |
|
Spasticity and contractures |
|
Deconditioning /muscle weakness |
|
Lowered mood |
|
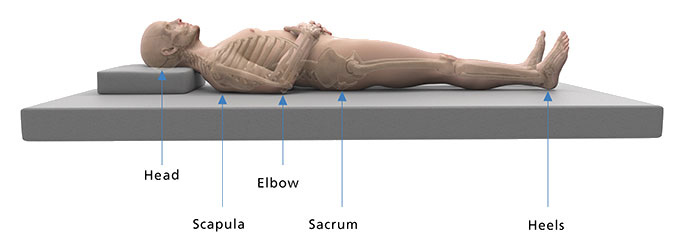
Bed positioning to remove pressure from the wound and protect other at-risk areas
Bed positioning to remove pressure from the wound and protect other at-risk areas
If the pressure injury is on the person’s bottom and/or contacts the sitting surface of the wheelchair, immediate 24 hour bed rest is usually required to remove or relieve pressure from the wound effectively. Identify the positions in which a person can lie so that there is no or minimal pressure on the wound and alternate between these positions in order to avoid prolonged pressure on another part of the body.
Monitor for complications of bed rest including respiratory complications and contractures.
Positioning in bed 20
Positions.20 Determine the range of positions in which the pressure injury/injuries are free from pressure using the SAMPLE Positioning Plan.
Mattress. Ensure the mattress is providing adequate pressure redistribution. Check areas of excessive pressure or possible ‘bottoming out’ on mattress by sliding hand between the person’s bony prominence and the mattress. Use a plastic bag as a glove to reduce friction and slide hand between the mattress cover and the mattress. If hand cannot easily fit through between the person’s body and the base of the mattress consider a different position and the need to ‘upgrade’ the mattress. Also refer to Manage Mechanical Factors: Mattress upgrade and selection in this Toolkit.
Prevent additional PIs. Protect all bony landmarks using cushions and positioning aids and consider precautions required in each position.
Prevent contracture. Use positioning aids and a range of motion program to prevent upper limb and lower limb contractures.
Repositioning. Reposition every 2-4 hours. Consider the use of slide sheets to change positions. Do not leave slide sheets or hoist slings in place under the person.
Trial. Trial any new position for 2 hours during the day and gradually increase to overnight depending on skin checks, comfort and safety.
Collaborate and communicate. Develop a practical and realistic positioning plan with the person and their carers. Display (if appropriate) and circulate the plan to carers with consent from the person.
Re-assess the positioning plan. Re-assess regularly, at least weekly, and check for complications such as deep venous thrombosis (DVT), pulmonary embolism (PE), pneumonia, secondary pressure areas, dehydration / malnutrition, contractures, deconditioning, muscle weakness, altered sleep patterns, psychological deterioration.
Refer to table: Preventing complications of bed rest in the above section “Minimise sitting and consider bed rest
Positions
Semi (30o) Side-lying

The semi (30o) side-lying position allows most bony landmarks to be free of pressure and avoids putting pressure directly on the greater trochanter (hip).20
Precautions
- Do not position directly on hip (GT) and shoulder
- Pillow or wedge behind back
- Pillow between legs and knees
- Position feet to protect bony prominences and minimise risk of contracture
- Consider placing top leg over bottom leg instead of on top of bottom leg if it does not increase pressure on the hip
Use wedges, pillows and positioning aids (avoid closed cut outs or doughnut-type cushions).
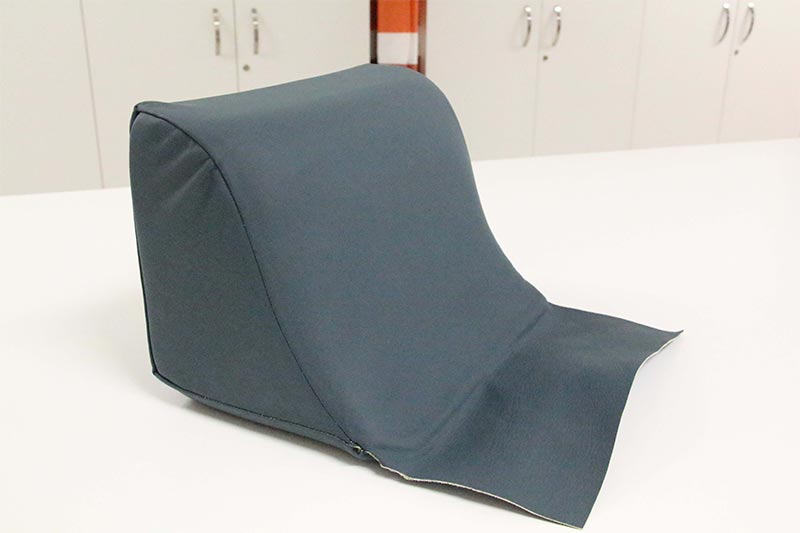 This is a side-lying wedge designed to support the 300 side lying position by removing pressure from the PI without increasing pressure on the weight-bearing shoulder and hip underneath.
This is a side-lying wedge designed to support the 300 side lying position by removing pressure from the PI without increasing pressure on the weight-bearing shoulder and hip underneath.It consists of layers of foam including a firm layer to provide support and a soft layer on the surface to provide pressure redistribution.
A Dartex cover and weldable seams are used for infection control.
Prone Lying

This position allows pressure to be completely removed from the ITs, GTs and Sacrum. The person can be supported with a combination of the following:
- Pillow under the abdomen to support lower back
- Pillow under chest/shoulders (e.g. two pillows in an inverted V or a boomerang pillow)
- Pillow under shins to raise toes off the mattress
- Prone face pillow to allow a face down position
- If using a hospital bed, use trendelenburg function to tilt the bed
Precautions
- Prone lying may not be possible for many people and it is not advised if it compromises respiratory function or is not safe.
- Consider liaising with the tertiary SCI and SB service to facilitate safe prone lying.
Supine
Precautions
- Ensure respiratory function is not compromised when lying flat or <30o.
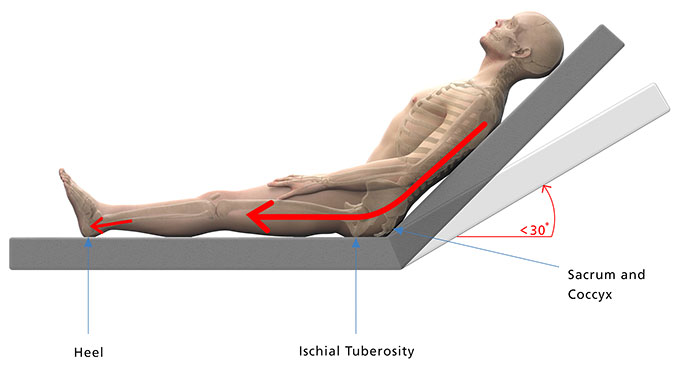
- To reduce shearing forces on the sacrum, avoid raising the bed head above 30o. Use the bed knee break to minimise sliding down the bed.
- Ensure the person’s heels are free from pressure and shearing forces.
Keep bed head at less than 30o

Ensure respiratory function is not compromised when lying flat or <30o.
Supine
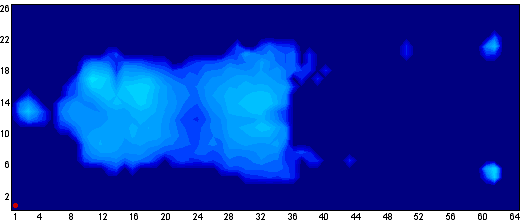
Pressure map of a person lying flat i.e. no head raise
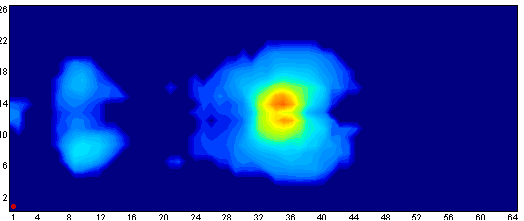
Supine with too much bed head raise
Pressure map of a person with the bed head raised past 30o
Offload the heels and prevent contracture

This heel wedge is designed to adequately lift the lower leg and free the heel from pressure without causing knee hyperextension which can cause popliteal vein obstruction (predisposing to DVT).
Products such as boots which lift the heel and support the foot in a neutral position may prevent contracture when the person is lying on their side. Ensure the device has maximum padding and can move with the person if the person experiences leg spasms.
A Dartex cover and weldable seams are used for infection control.
A pillow is positioned against the foot end of the bed here to prevent planter flexion contracture.
Mattress upgrade and selection
Mattress upgrade and selection
MATTRESS SELECTION
Static Support Surfaces
A static support surface is “a powered or non-powered support surface that changes its load distribution properties only in response to an applied load such as a person lying, sitting or moving on it11”. All mattresses except for alternating pressure mattresses fit into this category.
Consider a static support surface when:
- the person can be positioned without weight bearing on a PI, and
- without bottoming out on the support surface, and
- without developing red marks on their supporting side(s).
- Consider a low-air loss mattress to manage microclimate risks in addition to pressure.
Dynamic Support Surfaces
A dynamic (active) support surface is powered and has “the capability to change its load distribution with or without an applied load”. Alternating pressure mattresses use a powered pump that fills and deflates alternate air chambers over a set period of time. This allows pressure to be offloaded and redistributed during a cycle.
Consider a dynamic support surface if:
- the person cannot be positioned without pressure on the PI or
- when a static support surface bottoms out or
- if there is no evidence of healing or
- if red marks develop.
Key considerations when selecting and trialling a mattress20,11
In addition to a person’s individual pressure injury risk factors, below is a list of questions based on those provided in the Canadian Best Practice Guidelines for the Prevention and Management of Pressure Ulcers in People with SCI20 to guide the selection and trialling process.
Time
- What is the total and consecutive number of hours spent on the on the mattress?
- Will other pressure management strategies be able to be employed (frequent re-positioning, other effective pressure management equipment)?
- To determine if a mattress is appropriate, trial for short periods during the day and gradually increase the time depending on skin response until it matches the number of hours required overnight.
Pressure
- Does the mattress (i) redistribute pressure at high risk areas and (ii) adapt to weight fluctuation and positon changes?
- For static mattresses, look for (i) Immersion (the degree to which the mattress allows the body to ‘sink’ into it) and (i) Envelopment (the degree to which the mattress conforms to the contour of the body).
- Use the hand check to identify bottoming out or pressure mapping to compare mattresses. Bottoming out may occur in one mattress and not another in the same category.
- Interface pressure mapping (IPM) may be useful to compare two or more mattresses. Follow a standardised IPM protocol to ensure the comparison is accurate. If comparing alternating air mattress, pressure mapping should be recorded for the time it takes the mattress to complete a full cycle.
Microclimate
- Does the mattress (i) reduce or diffuse moisture and (ii) regulates / prevent an increase in temperature?
Friction
- Does it use smooth, friction-reducing fabrics?
Function and Lifestyle
- Are transfers, repositioning, dressing in bed and other activities safe when using this mattress?
- How does the mattress change the height of the bed and what impact will this have on transfers and carers?
- Active support surfaces are more unstable; however they may provide a higher level of pressure relief than more stable static mattresses.
Environment
- Does the partner need to be considered?
- Is the mattress compatible with the current bed, is a foam mattress surround required?
- Who will fund the mattress and what limitations are there? Use the Prescriber Guidelines provided by the funding body.
- Is it easy to operate?
Lifespan
- What is the mattress warranty and its expected lifespan? What are the possible maintenance requirements? Is an urgent replacement available if ever required?
Individual tolerance and risk
- Is it tolerated by the skin, comfortable, of preference to the client, noisy, does it contribute to dehydration (low air loss), does the person satisfy the safe work load (upper and lower limits) of the mattress?
- What is the person’s level of risk, number of pressure injuries? Refer to the Risk Stratification in this toolkit to identify specific risks.
- What is the goal of care (healable, non healable, maintenance or palliative)? How likely is the level of risk to change?
Safety issues
- Is there a risk of entrapment (check mattress is appropriate size) or falls?
- Is battery back up required? Is there a suitable power point?
- Does the person smoke in bed?
- Refer to the specific guidelines of the funding body for additional information required to justify mattress choice.
Implement a gradual return to sitting plan when appropriate
Implement a gradual return to sitting plan when appropriate
Implement a gradual return to sitting plan when appropriate
- The purpose of a gradual return to sitting plan is to incrementally increase pressure on the affected area by increasing the duration of the pressure, introducing additional movements or equipment one at a time and assessing the impact of each change.
- Not all PIs on the skin’s sitting surface are caused by sitting, however, pressure, friction, shear and microclimate when sitting can contribute to delayed healing or the skin breaking down again.
- A comprehensive Seating Assessment is required to “evaluate the person’s postural alignment, weight distribution, balance, stability and pressure-redistributing capability “.20
- Depending on pressure injury risk factors, the PI may need to be healed for a period of time before sitting can commence.
Establish an individualised return to seating plan that includes20:
- Safe transfers (may need to consider hoist, height adjustable bed and additional assistance in the short term until strength is regained and skin tolerance has improved).
- Effective pressure redistribution strategies (may need to consider power tilt in space wheelchair or shorter periods of sitting if the person is unable to weight shift effectively, i.e. offload pressure for 2 minutes every 15-30 minutes).
- A practical return to sitting plan (may require additional personal care to assist with more transfers and intervals of sitting). The plan is made in collaboration with the client and carers with respect to the amount of assistance that can be provided at home to implement the plan effectively.
- Other strategies which address risk across the 24 hour period including when to re- introduce and increase the use of commode, toilet, shower chair and car seat or downgrade a mattress for example.
- Skin check BEFORE and AFTER each session of sitting (take photos/video) to evaluate the skin’s response. Ensure the person and their carers can demonstrate knowledge of skin checking. Document skin changes on a Gradual Return to Sitting Plan.
- The process of returning to premorbid sitting time and activities (such as methods of transferring and equipment required) should be tailored to the individual.
- Inpatient or community rehabilitation should be considered if reconditioning is required and to implement changes and prevention strategies.
Optimise wheelchair positioning and support surface
Optimise wheelchair positioning and support surface
Review wheelchair support surfaces and ensure that the cushion provides:
- adequate pressure distribution over bony prominences,
- postural support and
- meets the functional needs of the individual.
CONSIDER20
- Magnitude and duration of pressure loading on each surface.
- Total contact area and weight bearing tolerance.
- Pressure re-distribution or off-loading capacity of the support surface.
- Effect of support surface on stability, balance and position (mobility and function).
- Potential of support surface to produce friction/shear.
- Durability and effectiveness.
- Maintenance requirements for continued effectiveness.
Ensure pressure redistribution strategies are effective
Ensure pressure redistribution strategies are effective
- Regular pressure re-distribution strategies help to reduce pressure over vulnerable bony prominences and restore blood flow to tissues under load.
- A pressure relieving position should be sustained for at least 2 minutes to restore blood flow to the area and performed every 15 – 30 minutes.
- Regular active movement, habitual re-positioning in the wheelchair and purposeful active weight shifts are all helpful to alleviate pressure if they do not present shear or friction risks to fragile skin.
- Traditional “pressure lifts” can be replaced with forward and side to side leaning to reduce strain on shoulders and wrists.
- There may be a need to consider a power tilt in space wheelchair for people who are unable to independently perform an effective weight shift.
- If using tilt-in-space in a powered wheelchair, tilting more than 30 degrees is required to adequately relieve pressure off the person’s bottom.
Sitting upright in wheelchair 
Corresponding pressure map of bottom
(i) Sitting upright 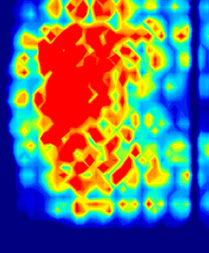
Forward-leaning weight shift 
(ii) Forward lean 
Image credit: NSW Spinal Outreach Service
Sitting upright in wheelchair 
Side-leaning weight shift 
Angle of tilt required to relieve pressure on ischial tuberosities. 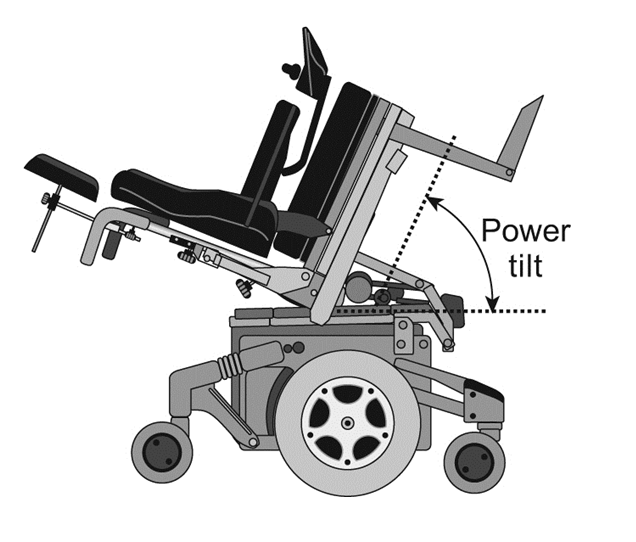
Optimise all other support surfaces
Optimise all other support surfaces
- Use a pressure redistributing surface on the commode/toilet or shower seat
- Optimise bowel care routine to minimise time sitting on a commode/toilet
- Consider transfer techniques, posture, stability, methods of bowel care and bladder emptying and assistance required.
- Even if the commode/ toilet or shower seat was not the original cause of the PI, inadequate pressure care on these support surfaces can contribute to delayed healing or recurrence of a PI on the ITs, sacrum, coccyx and GTs.
Wound Location

- Prolonged pressure from long periods of sitting on the commode seat or an inadequate commode seat can result in a PI on the underside of the Greater Trochanter (pictured here).
- PIs can develop on other parts of the bottom due to friction when transferring or repositioning on a commode or toilet seat.
- Poor posture or incorrect positioning on the commode can result in a sacral PI.
- Extreme care must be taken by carers when re-positioning the person on the commode.
Features of a commode seat
Features of a commode or toilet seat that will optimise pressure distribution, reduce friction and shear risks and maximise function include:
- Hand stitched seam on the underside of the seat
- Deluxe foam padding wrapped around aperture
- Custom cut out (“bite”) for independent bowel care or specified opening if required
- 4-Way stretch vinyl to allow some immersion into the foam

Referral to an Occupational Therapist and consultation with a SCI and SB – specific OT or Seating Therapist is recommended to ensure customisations are appropriate.
Reference
1. Houghton, Campbell et al 2013 p.164
Address contributing psychosocial and lifestyle factors and impact of a PI
For the pressure injury management plan to be effective and short term, it takes priority over all other activities and commitments.
Immediate social, practical and psychological support is critical to the success of treatment, particularly if it involves bed rest11. Most people with a pressure injury will need additional assistance to complete activities of daily living2.
Identify competing priorities and devise and re-evaluate practical strategies by adopting a Lifestyle-focussed approach to pressure injury management and prevention.
Lifestyle-focussed approach
Providing information alone may not be adequate to help people with SCI to manage and prevent pressure injury. The effectiveness of pressure management strategies may rely on the extent to which they have been ‘built-in’ to a person’s routine and habits.
The Lifestyle Redesign® for Pressure Ulcer Prevention in Spinal Cord Injury project (University of Southern California (USC) and Rancho Los Amigos National Rehabilitation Center (RLANRC) identified the need for highly individualised interventions to target and change lifestyle factors related to pressure injury development8,16,54.
Key concepts8,16,54
- A broad range of lifestyle factors should be addressed (See Lifestyle Factors table found in Assessment: More information on psychosocial and lifestyle factors in this Toolkit) and the idea that risk compounds in some situations should be acknowledged.
- The approach is highly individualised and tailored. Interventions are specific to the person, their unique circumstances and individual differences.
- The aim is to facilitate a person’s ability to implement sustainable strategies and responses into their lives through motivational interviewing, coaching and skill mastery.
- Strategies must be practical and realistic given the life circumstances experienced by some people.
- For the health professional, solutions are time intensive and highly involved. Interventions are delivered face to face and by telephone over an extended period of time.
Explore the person’s pressure injury experience and responses to a PI to identify barriers to wound healing .
Pressure injury experience and responses to a PI to identify barriers to wound healing
It is important to know if this is the first major pressure injury that the person has experienced or if it is a recurrent problem that they are trying to manage.
Langemo et al 2000 used the following themes to describe the pressure injury experience20:
- Cause of pressure injury
- Impact on life
- Psychospiritual impact
- Pain
- Need for knowledge
- Experience of stressful interventions
- Grieving process
| Responses to a PI which may interfere with healing | |
|---|---|
| Lacking knowledge | Inability to:
|
| Procrastinating | Delays seeking medical attention due to:
|
| Cognitive impairment | Inadequate response due to
|
| Diverting attention |
|
| Avoiding social discomfort |
|
| Being disillusioned by inadequate medical help |
|
| Relying on self/caregiver help |
|
| Adhering to medical recommendations |
|
- Promote self management
- Involve a Social Worker and/or Psychologist (and Psychiatrist particularly if there are pre-existing mental health problems)
- Access peer support
- Educate family and friends to support and motivate