Mount Druitt Medical Centre
In 2013, Mt Druitt Medical Centre had three doctors and two receptionists working in its clinic. The clinic didn’t measure their outcomes, and there was no plan for the clinic's culture. It ran as a very doctor-centric practice.
The decision to change this was inspired by the Royal Australian College of General Practitioner’s paper, Quality general practice of the future, published in 2012.
The centre installed Pen CAT, a software program that allowed them to review and analyse data they were already collecting. The data provided a new way to look at the practice population, patient outcomes and patient requirements. It gave the centre insight into population needs, and a view as to what care would be needed in future.
Using the data, the centre was able to identify that psychology, exercise physiology and dietetics were areas that required focus. They engaged clinicians to co-locate within the centre to work as an integrated team, increasing the amount of services they could offer in a targeted, reasoned way.
When these changes began, staff turnover was high, and it was a challenge to recruit staff members who were a good fit for the practice. An ongoing challenge is finding ways to ensure the staff work well as a team.
The centre's current system for supporting stronger teamwork involves:
- weekly meetings of the clinical team
- fortnightly meetings of the clerical team
- monthly meetings of the entire staff
- monthly meetings of clinical and relevant clerical staff for data review.
The clinic connects with the healthcare neighbourhood by including local chronic disease management staff at their weekly case conferences.
Monthly data meetings are held to review and analyse the Pen CAT data collected, and determine areas of focus for the upcoming month. In a given month, for example, staff may focus on patients with hypertension, and review how many of these patients have had their blood pressure taken in recent visits. The clerical staff can then coordinate the care for the patients who haven’t visited in a specified time by making appointments for them. A data manager within the practice spends 1 day a week running searches and analysing results of their system's data.
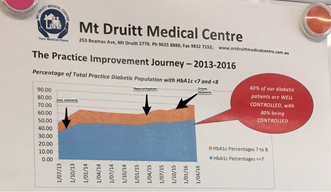
An example of data collected and how this informs practice, displayed in the staff room.
The clinic also upskills its staff and uses all staff members as part of the care team by envisioning the potential roles staff members can play, rather than just those they do play. For example, the clinic dietician has been trained to write up and review care plans for patients, which are then reviewed jointly by the dietician, patient and general practitioner. All allied health staff at Mt Druitt Medical Centre are engaged on individual contracts.
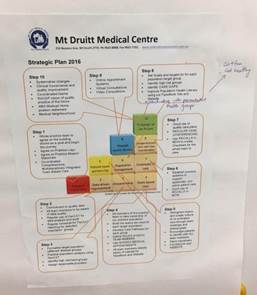
The 10 building blocks of high-performing primary care(1) have become the way business is done at Mt Druitt Medical Centre. Their strategic plan is a living document, formulated around these building blocks. The centre displays this plan for all staff to see, along with printed copies of charts to allow staff to track the progress of their patients and consider the effectiveness of the care they provide.

Implementing patient centred medical home principles has also allowed for a staged, comprehensive approach to the management of the centre’s patients. For example, a patient who presents with poorly-managed bipolar disorder, diabetes, chronic obstructive pulmonary disease and asthma can have their conditions prioritised and dealt with holistically. First, this patient would have their mental health issue vigorously targeted, while less intensive management of their other conditions takes place. Once their bipolar disorder is under control, the patient is in a better position to self-manage their physical conditions.
Since they transitioned to incorporate patient centred medical home principles into their practice, the Mt Druitt Medical Centre staff are happier and work with a sense of purpose.
References
- Bodenheimer T, Ghorob A, Willard-Grace R et al. The 10 building blocks of high-performing primary care. Annals of Family Medicine 2014; 12(2):166-171.


