Pressure Injury Toolkit For Spinal Cord Injury and Spina Bifida
Beyond the wound - Bringing best practice to the bedside

Bed positioning to remove pressure from the wound and protect other at-risk areas
If the pressure injury is on the person’s bottom and/or contacts the sitting surface of the wheelchair, immediate 24 hour bed rest is usually required to remove or relieve pressure from the wound effectively. Identify the positions in which a person can lie so that there is no or minimal pressure on the wound and alternate between these positions in order to avoid prolonged pressure on another part of the body.
Monitor for complications of bed rest including respiratory complications and contractures.
Positioning in bed 20
Positions.20 Determine the range of positions in which the pressure injury/injuries are free from pressure using the SAMPLE Positioning Plan.
Mattress. Ensure the mattress is providing adequate pressure redistribution. Check areas of excessive pressure or possible ‘bottoming out’ on mattress by sliding hand between the person’s bony prominence and the mattress. Use a plastic bag as a glove to reduce friction and slide hand between the mattress cover and the mattress. If hand cannot easily fit through between the person’s body and the base of the mattress consider a different position and the need to ‘upgrade’ the mattress. Also refer to Manage Mechanical Factors: Mattress upgrade and selection in this Toolkit.
Prevent additional PIs. Protect all bony landmarks using cushions and positioning aids and consider precautions required in each position.
Prevent contracture. Use positioning aids and a range of motion program to prevent upper limb and lower limb contractures.
Repositioning. Reposition every 2-4 hours. Consider the use of slide sheets to change positions. Do not leave slide sheets or hoist slings in place under the person.
Trial. Trial any new position for 2 hours during the day and gradually increase to overnight depending on skin checks, comfort and safety.
Collaborate and communicate. Develop a practical and realistic positioning plan with the person and their carers. Display (if appropriate) and circulate the plan to carers with consent from the person.
Re-assess the positioning plan. Re-assess regularly, at least weekly, and check for complications such as deep venous thrombosis (DVT), pulmonary embolism (PE), pneumonia, secondary pressure areas, dehydration / malnutrition, contractures, deconditioning, muscle weakness, altered sleep patterns, psychological deterioration.
Refer to table: Preventing complications of bed rest in the above section “Minimise sitting and consider bed rest
Positions
Semi (30o) Side-lying

The semi (30o) side-lying position allows most bony landmarks to be free of pressure and avoids putting pressure directly on the greater trochanter (hip).20
Precautions
- Do not position directly on hip (GT) and shoulder
- Pillow or wedge behind back
- Pillow between legs and knees
- Position feet to protect bony prominences and minimise risk of contracture
- Consider placing top leg over bottom leg instead of on top of bottom leg if it does not increase pressure on the hip
Use wedges, pillows and positioning aids (avoid closed cut outs or doughnut-type cushions).
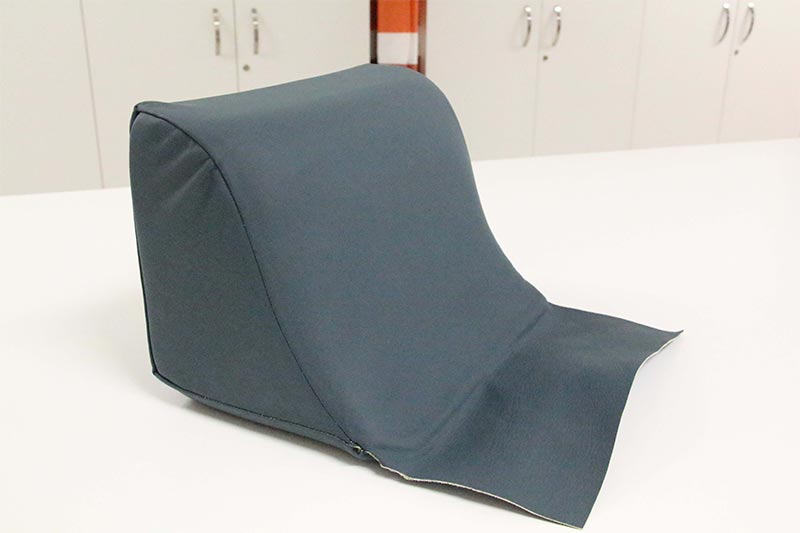 This is a side-lying wedge designed to support the 300 side lying position by removing pressure from the PI without increasing pressure on the weight-bearing shoulder and hip underneath.
This is a side-lying wedge designed to support the 300 side lying position by removing pressure from the PI without increasing pressure on the weight-bearing shoulder and hip underneath.It consists of layers of foam including a firm layer to provide support and a soft layer on the surface to provide pressure redistribution.
A Dartex cover and weldable seams are used for infection control.
Prone Lying

This position allows pressure to be completely removed from the ITs, GTs and Sacrum. The person can be supported with a combination of the following:
- Pillow under the abdomen to support lower back
- Pillow under chest/shoulders (e.g. two pillows in an inverted V or a boomerang pillow)
- Pillow under shins to raise toes off the mattress
- Prone face pillow to allow a face down position
- If using a hospital bed, use trendelenburg function to tilt the bed
Precautions
- Prone lying may not be possible for many people and it is not advised if it compromises respiratory function or is not safe.
- Consider liaising with the tertiary SCI and SB service to facilitate safe prone lying.
Supine
Precautions
- Ensure respiratory function is not compromised when lying flat or <30o.
- To reduce shearing forces on the sacrum, avoid raising the bed head above 30o. Use the bed knee break to minimise sliding down the bed.
- Ensure the person’s heels are free from pressure and shearing forces.
Keep bed head at less than 30o

Ensure respiratory function is not compromised when lying flat or <30o.
Supine
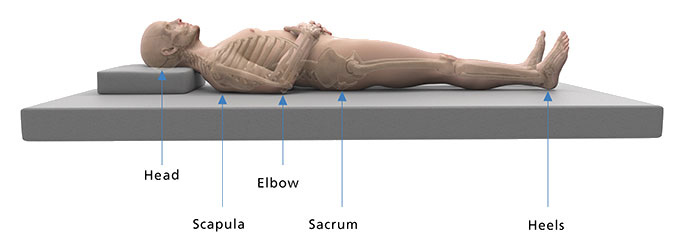
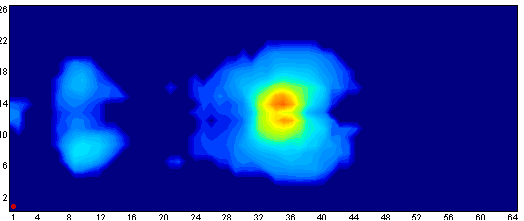
Pressure map of a person lying flat i.e. no head raise
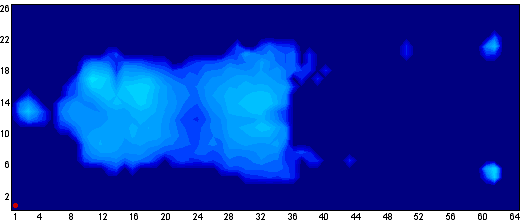
Supine with too much bed head raise
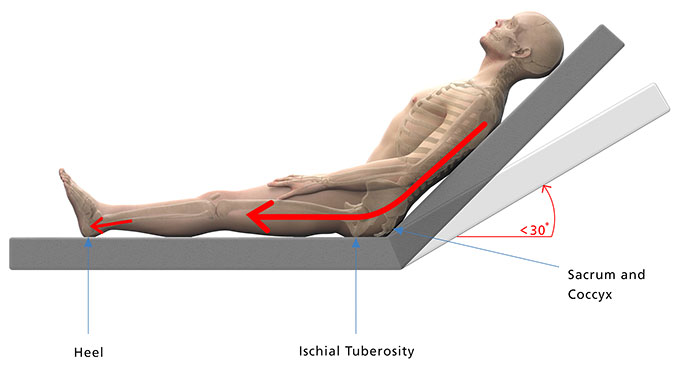
Pressure map of a person with the bed head raised past 30o
Offload the heels and prevent contracture

This heel wedge is designed to adequately lift the lower leg and free the heel from pressure without causing knee hyperextension which can cause popliteal vein obstruction (predisposing to DVT).
Products such as boots which lift the heel and support the foot in a neutral position may prevent contracture when the person is lying on their side. Ensure the device has maximum padding and can move with the person if the person experiences leg spasms.
A Dartex cover and weldable seams are used for infection control.
A pillow is positioned against the foot end of the bed here to prevent planter flexion contracture.