Foot and Ankle Injuries
Distal Tibia and Fibia
Summary
The ankle joint (talocrural joint) is a synovial hinge type joint. It is formed by the fibula, tibia and talus. The distal ends of the fibula and tibia form a socket known as the mortise in which the talus sits. A complex series of ligaments support the joint. The main movements of the joint are plantarflexion and dorsiflexion. In plantarflexion it is possible for some rotation, abduction and adduction movements. The joint is more stable in dorsiflexion than plantarflexion.
Fractures of the distal tibia and fibula may result in loss of stability of the ankle joint. They may present as a fracture only, fracture and ligamentous injury, multiple fractures or a fracture dislocation.
Fracture Type | Management | Follow-up |
|---|---|---|
Isolated lateral malleolus | Weber A: walking cast or boot, WBAT Weber B, undisplaced: short leg backslab NWB Weber B, displaced: short leg backslab, NWB | Orthopaedic follow-up in 7-10 days Orthopaedic follow up in 7-10 days Orthopaedic follow-up in ED or within 1-2 days |
Fibula fracture above syndesmosis (Weber C) | Ankle in normal anatomical position: short leg backslab NWB Talar shift or medial malleolar fracture: reduction, short leg backslab | Orthopaedic follow-up in ED or within 1-2 days Orthopaedic follow-up in ED |
Isolated medial malleolus | Short leg backslab, NWB | Orthopaedic follow-up in 7-10 days |
Bimalleolar and bimalleolar equivalent | Reduction if required, short leg backslab, NWB | Orthopaedic review in ED |
Posterior malleolus | Undisplaced/ Displaced/>25% of articular surface: short leg backslab, NWB | Orthopaedic review 7-10 days Orthopaedic review either in ED or within 1-3 days. |
Fracture dislocation | Reduction, Short leg backslab | Orthopaedic review in ED |
Open Fractures | Wound cleaned Manage based on fracture type | Orthopaedic review in ED |
Classification
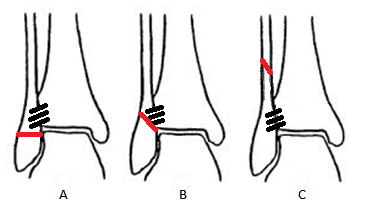
Danis-Weber classification
Based on the position of the fibular fracture. Higher risk of syndesmotic disruption and instability is associated with more proximal fractures.
Weber A - a fibular fracture below the level of the syndesmosis. Mechanism is supination of the foot.
Weber B - a fracture at or near the level of the syndesmosis. Mechanism is external rotation of the foot. May be associated with medial ankle injury/fracture or posterior malleolus fractures.
Weber C - a fracture above the level of the syndesmosis. Causes disruption of the syndesmosis and is usually associated with medial ankle injuries. This type of injury includes Maisonneuve injuries.
Lauge-Hansen classification:
Based on foot position at time of injury and the force applied through the foot.
- Supination-Adduction
- Supination-External Rotation
- Pronation-Abduction
- Pronation-External Rotation
Anatomical classification:
- Isolated lateral malleolus
- Isolated medial malleolus
- Bimalleolar
- Trimalleolar
- #/dislocation
Presentation
Presentation may vary between patients. From weight bearing with an antalgic gait to non-weight bearing with significant pain, swelling, discomfort and varying deformity.
Neurovascular status should be carefully examined.
The skin should be assessed for any open injuries and the amount of soft tissues swelling.
Dislocations should be reduced and casted immediately.
The patient should be assessed for:
- Swelling
- Deformity
- Open injuries
- Site of tenderness (palpate entire length of fibula)
- Other injuries
- Time since injury
- Weight bearing status
- Neurovascular status
- Related PMHx.
Imaging
X-ray: AP, lateral and mortice views.
ED Management Options
- Fracture dislocations should be reduced
- Open wounds should be cleaned and dressed in a sterile manner
- The leg should be elevated
Lateral malleolar fractures:
The stability of a fibula fracture determines treatment. Fractures distal to the syndesmosis are unlikely to be associated with ligamentous injury and therefore likely to be stable.
Fibula fractures that are associated with medial fractures or medial ligamentous injury are likely to be unstable despite normal alignment on x-ray. Talar shift or widening of the mortice indicates instability.
Fractures below the syndesmosis (Weber A avulsion type injuries) without associated medial ankle #/tenderness can be treated in a walking/CAM boot and may mobilise WBAT.
Isolated fibular fractures at the level of the syndesmosis (Weber B) without associated medial injury should be placed in a short leg backslab (ankle at plantargrade) and remain NWB.
Fractures above the syndesmosis (Weber C) involve disruption of the syndesmosis and are usually associated with medial ankle injury. These fractures should be placed in a short leg backslab and remain NWB.
Fibular fractures which are displaced >3mm, have associated medial malleolar fracture or medial ligament injury are unstable and require orthopaedic review. A short leg backslab, ankle at plantargrade, should be applied. NWB mobility.
Medial malleolus fractures:
With medial malleolus fractures care should be taken to rule out any other fracture or injury around the ankle. The entire length of the fibula should be palpated and x-rayed to rule out any Maisonneurve type injuries. Any other fracture, ligament injury or talar shift indicate the fracture is likely to be unstable and should be reviewed by orthopaedics.
If medial malleolar injury is truly isolated then a short leg backslab should be applied and the patient is to remain NWB until orthopaedic review.
Bimalleolar/trimalleolar
These fractures are unstable and require ORIF. A short leg backslab should be applied. NWB
Posterior malleolus
As with medial malleolar fractures care should be taken to rule out any other injury about the ankle which would indicate instability.
Fractures that involve >25% of the articular surface or a displaced >2mm usually require an ORIF. CT is the best way to determine articular displacement.
A Short leg backlsab should be applied, NWB mobility, for all posterior malleolus fractures.
Fracture dislocation
Reduction, short leg backslab, elevate. Requires orthopaedic review and ORIF. NWB.
Open Fractures
Clean and dress wound, short leg backslab. Orthopaedic review.
Referral and Follow Up Requirements
Fracture Type | Urgency | Follow-up |
|---|---|---|
Isolated lateral malleolus | Undisplaced: non- urgent Displaced: urgent | Orthopaedics 7-10 days Orthopaedics in ED or within 1-2 days. |
Isolated medial malleolus | Undisplaced: non-urgent Displaced: urgent | Orthopaedics 7- 10 days Orthopaedics in ED or within 1-2 days |
Bimalleolar and bimalleolar equivalent | Urgent | Orthopaedic review in ED |
Posterior malleolus | Displaced: urgent Undisplaced: non urgent | Orthopaedic review in ED or within 1-2 days Orthopaedic review 7-10 days |
Fracture dislocation | Urgent | Orthopaedic review in ED |
Open Fractures | Urgent | Orthopaedic review in ED |
Potential Complications
Non-union is rare. Malunion may occur with a lateral malleolus fracture that is shortened or rotated, a displaced posterior or medial malleolus fracture or a talar shift.
Arthritic changes can occur due to damage at time of injury or malunion.
Patient Advice
Pain from the fracture and restriction of movement is usual for 2-3 weeks and will require regular, then prn analgesia
Monitor for compartment syndrome
Further References and Resources
- Koval, K & Zuckerman, J (2002) Handbook of fractures, Philadelphia: Lippincott Williams and Wilkins
- Orthobullets - ankle fractures
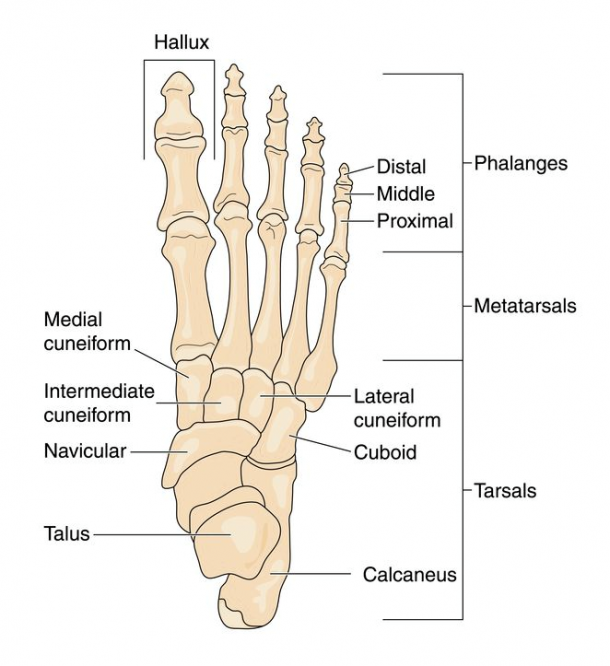
Navicular and Cuboid Injuries
Summary
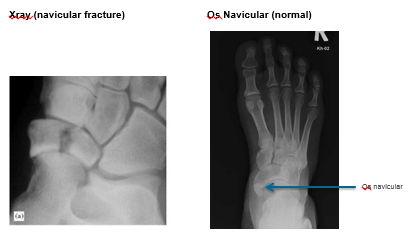
Most isolated midfoot fractures affect the navicular or more rarely the cuboid bones. The majority consist of minor avulsion or stress fractures. Significantly displaced fractures often require orthopaedic intervention. The navicular bone is particularly at risk for avascular necrosis, difficult to diagnose, and therefore a high index of suspicion is required to identify this injury.
Classification
Sangeorzan Classification of Navicular Body Fractures
Type 1: coronal fracture with no dislocation.
Type 2: dorsolateral to plantomedial fracture with medial forefoot displacement.
Type 3: comminuted fracture with lateral forefoot displacement and carries the worst prognosis.
Epidemiology
Because navicular stress fractures are not easily observed on plain radiographs, the reported incidence rates vary widely. The overall incidence may appear to be increasing due to advances in imaging.
There is limited epidemiology data related to cuboid and navicular fractures. Some reports estimate that cuboid fractures represent approximately 50% of midfoot fractures, with navicular fractures making up approximately 40%.
Presentation
Mechanism
Stress fractures should be considered in any athlete with midfoot pain.
Traumatic fractures may result from a fall from a height if the foot hits the ground in a plantar-flexed position. This may result in transmitting axial and rotatory forces along the lateral midfoot and hindfoot. Avulsion injuries can also occur with a pulling or rotational force (e.g. eversion forces) from horseriding and sports activities.
In most instances, navicular and cuboid fractures are associated with significant fractures to the talus, calcaneus, or tarsometatarsal region. Take care to exam all areas of the foot and ankle.
These fractures typically occur with pain, swelling and bruising over the relevant anatomical area.
Imaging
Use Ottawa X-ray Rule for those with foot and ankle injuries for determining who needs acute imaging.
Plain film radiographs (X-rays) including AP, lateral and oblique foot and ankle X-rays.
If initial radiographs are negative and the patient remains significantly tender or non-weight bearing; discuss with senior ED clinician or orthopaedic registrar/consultant as CT scanning may be required.
ED Management Options
Fracture Type | Treatment | Referral |
|---|---|---|
Navicular Type 1 and 2 | Below knee POP backslab Non weight bearing Analgesia, elevate | Orthopaedic surgeon review in 1 week |
Navicular Type 3 | Below knee POP backslab Non weight bearing Analgesia, elevate | Refer to orthopaedic surgeon in ED – likely admit for ORIF |
Cuboid Fractures | Below knee POP backslab Non weight bearing Analgesia, elevate | Discuss with orthopaedic surgeon about treatment and follow up |
Potential Complications
Complications of navicular and cuboid injuries include:
a. Avascular necrosis (AVN)
b. Non-union and
c. Instability
d. Osteoarthritis/arthrosis
All of which can lead to a flatfoot deformity and pain.
Patient Advice
General health advice (smoking cessation, controlling diabetes etc.) needs emphasis as these conditions have higher association with complications and delayed union.
Non-weight bearing needs to be emphasised as these fractures (particularly the navicular) are prone to avascular necrosis and non union. The exception are avulsion flake fractures where the patient is permitted to weight bear but only on the advice of an orthopaedic surgeon.
For stable injuries:
- Follow up with an orthopaedic surgeon within 1 week.
- CT or MRI may be required to further investigate this injury if the patient has ongoing pain and swelling.
- Pain from the fracture and restriction of movement is usual for 2-3 weeks and will require regular, then prn analgesia.
- Monitor for compartment syndrome.
- ECI patient factsheets
Further References and Resources
- Orthobullets - tarsal navicular fractures.
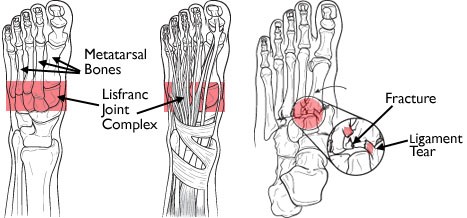
Lisfranc Injuries
Summary
Injuries to the Lisfranc joints are uncommon but can be difficult to diagnose. A high degree of suspicion for lisfranc injuries must be maintained for all patients presenting with midfoot pain and swelling and a significant mechanism. X-rays often do not reflect the extent of the injury and CT is necessary to show the significant bony and ligamentous disruption that characterises this injury. Missed lisfranc injuries result in significant post traumatic arthritis.
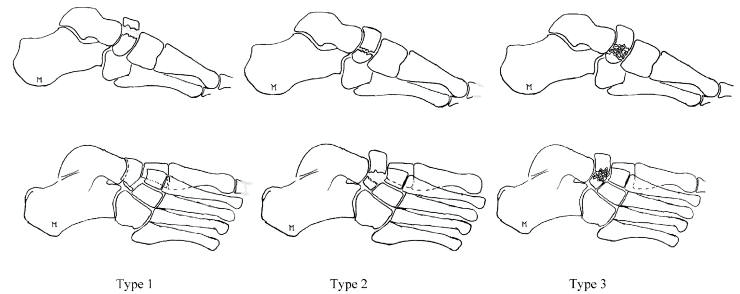
Classification
There are several classification systems for TMTC injuries.
The most commonly used classification is that developed by Quene and Kuss in 1909:4
- Homolateral: All five metatarsals displaced in the same direction.
- Isolated: One or two metatarsals displaced from the others.
- Divergent: Metatarsals are displaced in both the sagittal and coronal planes.
The above system was further modified by Myerson et al. in 1986 to the following which gives much more anatomical detail.1
- Type A total incongruity of the TMT joint.
- Type B injuries – partial Incongruity
- Type B1 partial incongruity affecting the first ray in relative isolation (i.e. partial medial incongruity);
- Type B2 partial incongruity in which the displacement affects one or more of the lateral four MTs (i.e. partial lateral incongruity).
- Type C - Divergent
- Type C1 Partial displacement
- Type C2 total displacement.
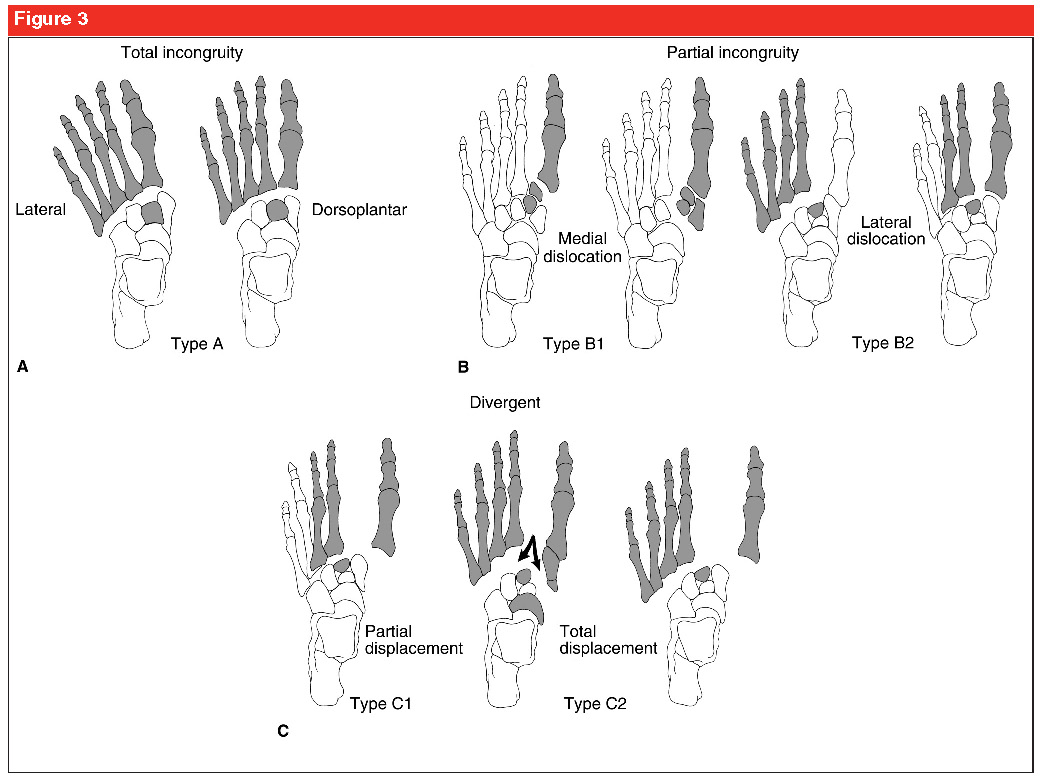
Classification of tarsometatarsal joint injury. The shaded areas represent the injured or displaced portion of the foot.
- A, Type A, total incongruity, which involves displacement of all five metatarsals (MTs) with or without fracture at the base of the second MT. The usual displacement is lateral or dorsolateral, and the MTs move as a unit. These injuries are “homolateral.”
- B, In type B injuries, one or more articulations remain intact. Type B1 represents partial incongruity with medial dislocation. Type B2 represents partial incongruity with lateral dislocation; the first MT cuneiform joint may be involved.
- C, Type C injuries are divergent, with either partial (C1) or total (C2) displacement. The arrows in C2 represent the forces through the foot leading to a divergent pattern.
Redrawn with permission from Myerson MS, Fisher RT, Burgess AR, Kenzora JE: Fracture-dislocations of the tarsometatarsal joints: End results correlated with pathology and treatment. Foot Ankle1986;6:225–242.
Epidemiology
- First described by Jacques Lisfranc de St Martin (1790-1847), a field surgeon in the Naoleonic army. He described a significant injury to the MTC when a soldier fell off their horse with their foot in the stirrups. This caused a vascular injury, often requiring amputation through this joint.
- Uncommon injuries. Incidence in the USA is 1 per 55,000 people or 0.2% of all fractures (1).
- 1/3 are low velocity injuries – often sports related and involved forced plantarflexion with rotation or forced abduction.
- 2/3 are high velocity injuries with a similar mechanism, and result from motor vehicle and motorbike accidents, and falls from a height.
Presentation
- The Tarsometatarsal complex (TMTC) or lisfranc joint is made up of 9 bones - the 5 metatarsal bases, the proximal articular surfaces of the three cuneiforms and the cuboid laterally. Functionally it is the transition point between the forefoot and midfoot.
- The bases of the middle three metatarsals are trapezoidal in shape. Together with their associated cuneiforms, they form a transverse arch, the keystone of which is the second tarsometatarsal joint. This improves the inherent stability of this joint.
- The lisfranc ligament runs between the second metatarsal base and the medial cuneiform and is the strongest structure supporting the TMT complex. There are other ligamentous complexes that support the joint but the lisfranc ligament is the strongest.
Imaging
- Plain X-rays: AP, lateral and oblique films (with the image taken parallel to the midfoot 1). Up to 20% of injuries to the Lisfranc joint are missed on X-ray.
- Weight bearing views can make the deformity more obvious.
- The AP film shows malalignment of the 1st and 2nd tarsometatarsal joint, whereas the oblique film shows any malalignment at the 3rd and 4th tarsometatarsal joints.
- On the lateral view, the dorsal and plantar aspects of the MTs should correspond with the cuneiform and cuboid. A tangential line drawn through the medial aspect of the medial cuneiform and navicular should intersect the first MT base 1.
Any suspected TMTC injury should be further evaluated by a CT to assess the extent of the fractures and ligamentous injuries, particularly when the injury is sustained via a high energy mechanism. It is not uncommon for CT to show comminution and intraarticular extension of the fracture not seen on X-ray. CT may not show subtle displacement as it is also not a weight bearing test.
MRI will better evaluate the ligamentous and soft tissue injury aspect of the injury and is important in evaluation of the low energy injury subgroup in particular.
ED Management Options
- Adequate analgesia
- High index of suspicion based on clinical presentation and mechanism.
- Foot and ankle X-rays.
- CT if required.
- Orthopaedic consult to decide whether it is an unstable injury requiring an ORIF or a stable injury.
- Unstable Injuries:
- If any subluxation or ligamentous injury, lisfranc injuries require open reduction and internal fixation.
- Backslab, non weight bearing. Keep foot elevated. ADMIT for OT.
- Unstable Injuries – this will require immobilisation with a backslab and fixation in the operating theatre. Discharge planning and follow up will be as per the orthopaedic team.
- Stable injuries can be managed in a Cam Boot for 6-10 weeks, weight bearing as tolerated. Relative contraindications for surgical intervention may include insensate feet (e.g. charcot midfoot), inflammatory arthritis, nonambulatory status, and severe medical comorbidity.
Referral and Follow Up Requirements
Stable injuries – discharge in cam boot, weight bearing as tolerated. Follow up in 6 weeks.
Unstable injuries: Will have ORIF to restore anatomic alignment. Follow up to be determined by orthopaedic team.
Potential Complications
- Missed injury (up to 20% of injuries are missed initially).
- Post traumatic arthritis
- Ongoing foot pain and instability. May require salvage arthrodesis.
Patient Advice
- Stable injuries for discharge - weight bear as tolerated.
- Follow up with an orthopaedic surgeon within 2 weeks.
- You may require an MRI to further investigate this injury if you have ongoing pain and swelling.
- Pain from the fracture and restriction of movement is usual for 2-3 weeks and will require regular, then analgesia as required.
- Monitor for compartment syndrome.
- ECI patient factsheets
Further References and Resources
- Burge, A. et al. (2012) Imaging of Sports-Related Midfoot and Forefoot Injuries, Sports Health. 2012 Nov; 4(6): 518–534.
- Medscape -
- OrthoInfo - Lisfranc (Midfoot) Injury.
- Pyklawa T, Andersen,L; Midfoot Trauma, Current Orthopaedic Practice, 19(3), May 2008, p 228–233.
- Watson, T. et al. (2010) Treatment of Lisfranc joint injury: current concepts, J Am Acad Orthop Surg, December, 18(12), 718-28.
5th Metatarsal
Summary
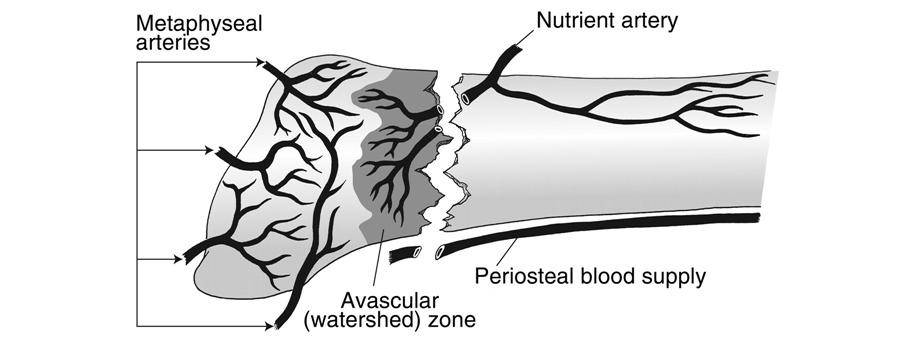
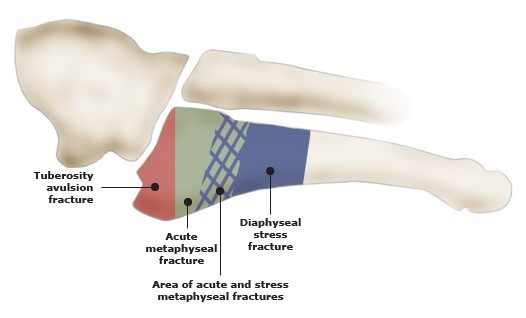
The proximal (base) 5th metatarsal can be divided into 3 sections - the tuberosity, metaphysis and diaphysis. The tuberosity articulates with the cuboid while the metaphysis articulates with the base of the 4th metatarsal. The intermetatarsal joints are plane type synovial joints that allow slight gliding movements. The lateral band of the plantar fascia attaches the base of the 5th metatarsal tuberosity. The peroneus brevis muscle, which everts the foot, attaches to the lateral tuberosity.
Blood supply to the proximal 5th metatarsal is via the metaphyseal arteries and nutrient artery. The metaphyseal arteries supply the tuberosity while the metaphysis and proximal diaphysis receive blood supply from the nutrient artery. Fractures of the metaphyseal/diaphyseal junction are therefore more likely to have problems with non-union.
Fracture Type | Management | Follow-up |
|---|---|---|
Tuberosity fracture | Walking boot for 4-6 weeks Weight bear as tolerated No running for 3 months | GP; 4-6 weeks post injury |
Acute metaphyseal/diaphyseal fracture | Short leg backslab Non weight bearing | Fracture clinic/orthopaedic follow-up within 7-10 days |
Proximal diaphyseal stress fracture | Short leg backslab Non weight bearing | Fracture clinic/orthopaedic follow-up within 7-10 days |
Classification
Based on anatomical location.
Presentation
Mechanism of injury
- Tuberosity fracture: inversion with foot in plantarflexion.
- Acute metaphyseal/diaphyseal fracture: forefoot adduction.
- Proximal diaphyseal stress fracture: repetitive microtrauma.
Assess
- Onset, duration and quality of pain.
- Palpate for area of tenderness.
- Weight bearing status (usually possible but painful).
- Neurovascular status.
- Evaluate surrounding structures.
Imaging
X-ray: AP, lateral and oblique foot views.
ED Management Options
Tuberosity Fracture:
- Walking boot (e.g. CAM boot) for 4-6 weeks as pain dictates, weight bear as tolerated.
- No running for 3/12.
Acute metaphyseal/diaphyseal fracture
- Short leg backslab (including toes), non-weight bearing.
Proximal diaphyseal stress fracture
- Short leg backslab (including toes), non-weight bearing.
Referral and Follow Up Requirements
Fracture Type | Urgency | Follow-up |
|---|---|---|
Tuberosity fracture | Non urgent | GP; 4-6 weeks post injury |
Acute metaphyseal/diaphyseal fracture | Non urgent | Fracture clinic/orthopaedic follow-up within 7-10 days |
Proximal diaphyseal stress fracture | Non urgent | Fracture clinic/orthopaedic follow-up within 7-10 days |
Potential Complications
Non or delayed union: especially with acute metaphyseal/diaphyseal and proximal diaphyseal fractures.
Patient Advice
Pain from the fracture and restriction of movement is usual for 2-3 weeks and will require regular, then analgesia as required
Further References and Resources
- Koval, K & Zuckerman, J (2002) Handbook of fractures, Philadelphia: Lippincott Williams and Wilkins.
- Orthobullets - 5th Metatarsal Base Fracture