Acute Liver Failure
Acute liver failure (ALF) is a rare syndrome defined by a rapid decline in hepatic function characterized by jaundice, coagulopathy (INR >1.5), and hepatic encephalopathy in patients with no evidence of prior liver disease. The interval from the onset of jaundice to the development of encephalopathy occurs within 24 to 26 weeks and may further classify ALF into categories based on hyperacute, acute, or subacute presentations. Although clinical jaundice is considered a defining feature of ALF, it may not always be present, particularly in hyperacute presentations.
Hyperacute liver failure
Presents within 7 days of onset. 36% survival with medical management alone.
Acute liver failure
Encephalopathy, coagulopathy and jaundice presenting within 8-28 days in patient with previously normal liver. More likely to get cerebral oedema (80%).
Subacute liver failure
Presents from 29-72 days, less likely to get cerebral oedema, but more likely to have ascites. Poorer 14% survival.
You may also want to view the Chronic Liver Failure (CLF) clinical tool.
Aetiology
Viruses e.g. Hepatitis A, E, B, HSV, CMV, EBV
Most common in developing world
Very poor survival in patients with reactivation Hep B with previously stable infection e.g. after immunosuppression treatment like chemo, steroids
Drugs
acetaminophen / paracetamol - most common in developed world
anticonvulsants - valproate (usually within first 6 months) or phenytoin (earlier usually within 2 months)
herbal supplements - e.g. kava, skull cap
See this link for all drugs and supplements implicated in liver injury
Other
Ischaemia / hypoxia e.g. after cardiac / respiratory arrest, sepsis
Neoplastic infiltration
Acute Budd Chiari syndrome (occlusion hepatic veins)
Heat stroke
Mushroom ingestion
Metabolic disease e.g. Wilsons
Pregnancy – acute fatty liver of pregnancy, HELLP syndrome
Idiopathic.
Signs and Symptoms
Clinical presentation usually includes hepatic dysfunction, abnormal LFTs and coagulopathy. Hepatic encephalopathy may develop along with multi-organ failure and death occurring in up to half of cases.
This diagram from Bernal and Wendo (2013) provides an overview of the clinical features of acute liver failure.
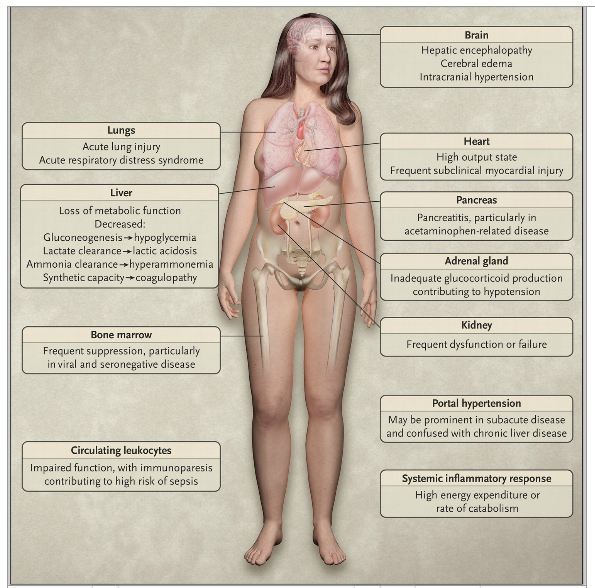
Source: Bernal, W. and Wendo, J. (2013) Acute Liver Failure, The New England Journal of Medicine, vol. 369, no. 26, pp. 2525 - 2534.
Investigations
- Bedside blood sugar
- Venous blood gas
- FBC: May reveal thrombocytopenia
- Coagulation studies
- Liver function tests: Often elevated levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP)
- Bilirubin level: Elevated
- Serum ammonia level: May be dramatically elevated. Risk of intracranial hypertension highest when sustained level ammonia 150-200µmol/L (250-340 µg/dl)
- Serum glucose level: May be dangerously low
- Lactate level: Often elevated
- Creatinine level: May be elevated
- Electrolytes: Na may be low, often dilutional due to fluid accumulation
- Calcium, magnesium, phosphate
- Paracetamol
- Blood cultures: For patients with suspected infection
- Pregnancy test
- Lipase
- CXR
- ECG
Tests to consider after consultation (dependent on clinical context)
- Viral serologies: Consider for hepatitis A virus immunoglobulin M (IgM), hepatitis B surface antigen (HBsAg), hepatitis B virus anticore IgM; hepatitis C viral load testing; hepatitis D virus IgM if HBsAg is positive; in posttransplantation or immunosuppressed setting, consider studies for cytomegalovirus viraemia and herpes simplex virus
- Autoimmune markers: Antinuclear antibody (ANA), anti-smooth muscle antibody (ASMA), and immunoglobulin levels
- Serum Copper
- Hepatic Doppler ultrasound
- CT Abdo
- CT Brain
- Echo: hypoxic hepatitis can result from myocardial dysfunction
Management
Management - general
- Restore intravascular volume early with IVF – may help mitigate / prevent multi-organ failure.
- May require inotropic support (Noradrenaline preferred).
- Use 0.9% saline as Hartmann's gives external lactate load and 5% dextrose may worsen hyponatraemia and hence cerebral oedema.
- N-acetylcysteine (NAC) – a RCT has found NAC can improve survival in patients with low grade encephalopathy (as well as in paracetamol).
- For non paracetamol poisoning regime similar to above (Lee et al. 2009) - refer to NAC protocol
- Regular neurological observations - patients may have rapid progression of encephalopathy / agitation/coma. Early intubation is recommended to protect airway (tip: maintain normocapnoea, PaCO2 35-45)
- Antibiotics (eg Ceftriaxone 1g) administered pre-emptively in patients with encephalopathy, evidence of infection / sepsis.
- Coagulation factors / Blood products should be avoided except if required to manage bleeding or before invasive procedures. Often there is a balanced loss of both hepatically derived procoagulant and anticoagulant factors. If bleeding can use FFP, platelets and/or recombinant factor VIIa. Early discussion with haematology advised.
- Maintain normoglycaemia - 50% dextrose infusion can be used in hypoglycaemic patients
- Maintain temperature 35-36°
- Stop offending drugs
- Early ICU involvement
- Please also see CLF tool for management of specific problems associated with liver failure eg ascites, GI bleeds, encephalopathy
- Some treatments used in CLF are inappropriate for use in ALF such as lactulose (can lead to aspiration), neomycin, rifaxamin (can lead to renal failure).
- Try to prevent intracranial hypertension consider sedation and use of osmotherapy
Management - specific
- HSV hepatitis
- aciclovir
- Acute fatty liver of pregnancy or HELLP syndrome
- expedient delivery of the fetus
- Suspected mushroom (Amanita phalloides) poisoning
- IV fluids + gastric lavage + activated charcoal
- benzylpenicillin
- acetylcysteine
- Autoimmune hepatitis
- methylprednisolone
- Acute hepatitis B
- oral nucleoside or nucleotide analogue
- Acute Budd-Chiari syndrome
- anticoagulation
- transjugular intrahepatic portosystemic shunt (TIPS)
- Acute Wilson's disease
- measures to decrease serum copper
Prognostic Evaluation
Important to identify potential candidates for transplantation. Indicators include presence encephalopathy, age, severity liver injury (coagulopathy/jaundice). ED will be involved in these decisions to some degree as we will flag these patients to gastroenterology, intensive care +/- retrieval and depending on the severity of their illness/encephalopathy, may need to make the decision to intubate them in the ED.
Disposition
Most / if not all patients will require HDU / ICU for management and monitoring
They may need referral to a Specialist Liver or Transplant Unit.
Further References and Resources
Bernal, W. and Wendo, J. (2013) Acute Liver Failure, The New England Journal of Medicine, vol. 369, no. 26, pp. 2525 - 2534
BMJ Best Practice – Acute Liver Failure
Lee, WM. et al. (2009) Intravenous N-Acetylcysteine Improves Transplant-Free Survival in Early Stage Non-Acetaminophen Acute Liver Failure, Gastroenterology, vol. 137, no. 3, pp. 856 - 864.