Sodium - Hyponatraemia
Key points
- A patient’s fluid status is key in determining the cause of hyponatraemia and dictating treatment
- The rate of correction of hyponatraemia should not exceed 8 mmol/L in 24 hours as over rapid correction can cause osmotic demyelination syndrome
- Hyponatraemic seizures and/or altered conscious state are a medical emergency and can cause irreversible neurological damage
Background
- Hyponatraemia is defined as serum sodium <135 mmol/L.
- Most patients with Na >125 mmol/L are asymptomatic.
- Hyponatraemia and rapid fluid shifts can result in cerebral oedema causing neurological symptoms.
- If Na <125 mmol/L or if serum sodium has fallen rapidly vague symptoms such as nausea and malaise are more likely and may progress.
- If severe hyponatraemia (Na <120 mmol/L): headache, lethargy, obtundation and seizures may occur.
- Chronic hyponatraemia (developing >24 hours) may have more subtle features such as restlessness, weakness, fatigue or irritability (due to cerebral adaptation)
- Rapid correction of hyponatraemia can result in osmotic demyelination syndrome which manifests as irreversible neurologic features (dysarthria, confusion, obtundation and coma) which often present days after sodium correction.
Causes of hyponatraemia:
Volume status | Cause hyponatraemia |
Hypovolaemia | Vomiting and/or diarrhoea Burns Diuretics (thiazides, indapamide, hydrochlorothiazide, chlortalidone) Hypopituitarism Primary adrenal insufficiency |
Euvolaemia | SIADH:
Hypothyroid Psychogenic polydipsia Secondary adrenal insufficiency |
Hypervolaemia | Heart failure Liver cirrhosis Kidney failure Nephritic syndrome |
Other | |
Pseudohyponatraemia | Severe hypertriglyceridaemia |
Osmotic dilution | Hyperglycaemia Mannitol administration |
Mechanism uncertain | HIV |
SIADH = syndrome inappropriate antidiuretic hormone secretion; SSRI = selective serotonin reuptake inhibitor; SNRI = serotonin and noradrenaline reuptake inhibitor
SIADH:
SIADH (Syndrome of inappropriate secretion of antidiuretic hormone) has several causes. These include cerebral or pulmonary pathology, drugs that can impair water excretion or malignancy.
If there is no diuretic or other obvious cause, SIADH is likely if the following results apply:
serum sodium concentration <130 mmol/L
serum osmolality < 275 mmol/kg
urine osmolality > 100 mmol/kg
urine sodium concentration > 30 mmol/L
Assessment
History consistent with common causes for hyponatraemia
History of fluid intake/losses
Clinical assessment of the patient’s current hydration status
Neurological status
Red Flags:
Nausea and vomiting
Irritability
Headache
Decreased conscious state
Seizures
Management
Investigations (recommended if Na <130 mmol/L)
- UEC
- Paired serum and urine osmolality
- Urinary sodium
- BSL (If hyperglycaemia present in addition to hyponatraemia see DKA/HHS)
- Consider blood gas if sick
- TFTs
- Random serum cortisol levels or adrenocorticotropic hormone stimulation test - Considered in suspected adrenal suppression (e.g. recent steroid use).
Treatment
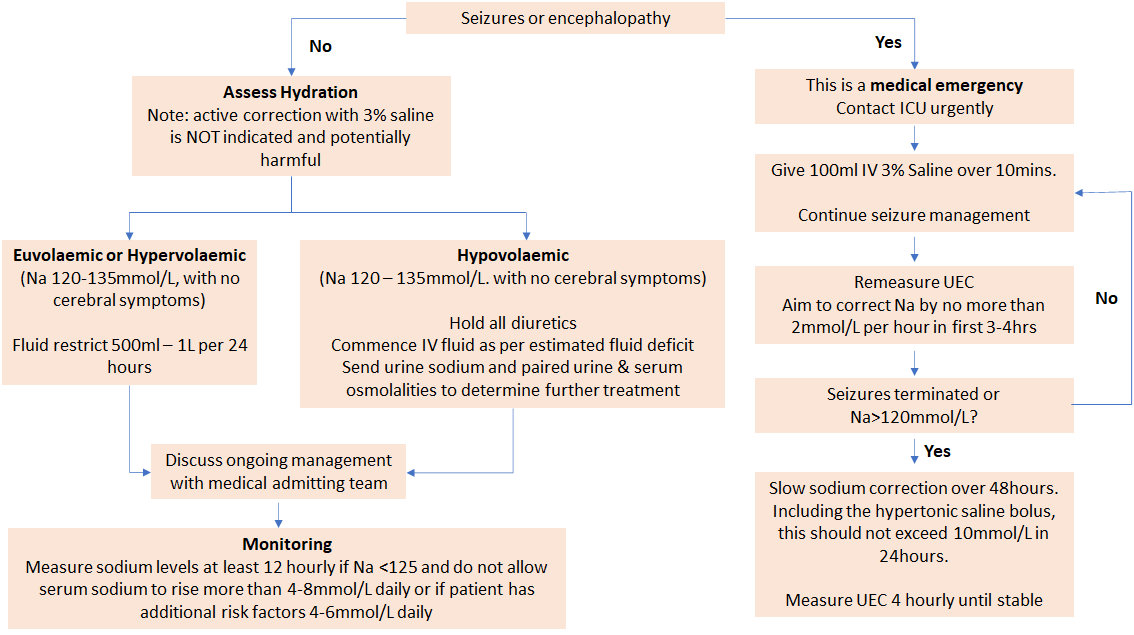
- Management is determined by presence of seizures/ altered conscious state and fluid status (see flow chart below).
- The target rate of serum sodium correction is 4-8mmol/L in 24 hours (unless seizing- see flow chart below).
- If additional risk factors (Na < 105 mmol/L, hypokalaemia, alcoholism, malnutrition, advanced liver disease), advise aim of rate of correction should be 4 – 6 mmol/L daily.
- All patients should have a strict fluid balance including weight (minimum daily, but maybe 6-12 hourly for more unwell patients).
- Remember to treat the underlying cause.
Hyponatraemia treatment flowchart:
*Notes
Risk of morbidity from delayed treatment is greater than the risk of osmotic demyelination from overly rapid correction. Therefore, aggressive initial correction is indicated for the first 3-4 hours (or until symptoms resolve) at a rate not to exceed 2 mmol/L per hour
Hyponatraemic seizures may be refractory to anticonvulsants and sodium correction should not be delayed
Maximum 3 infusions of 3% Saline
3% Saline should preferably be given via a central line
Consider consultation with critical care team when
The patient has had CNS symptoms including seizures or altered conscious state