The Very Intensive Patient (VIP) program is an innovative strategy that integrates care inclusively and collaboratively across primary, secondary and tertiary healthcare. The program partners with social care providers to maximise the efficiency of care coordination, and formally assesses client needs in line with evidence‐based risk factors for representation or readmission to hospital.
Aim
To identify people at high risk of repeat presentation to the emergency department (ED) and/or risk of unplanned readmissions to hospital; the aim is to improve a person’s quality of life and healthcare experience by addressing their social determinants of health.
Benefits
Patient benefits
- Improved healthcare journey and patient experience.
- Development of individualised care plans that meet person-centred needs.
- Focus on wellbeing and improved quality of life.
Staff benefits
- Reduced staff burnout by empowering staff to implement changes that impact care.
- Cultural change to decrease negative labelling and removing term “frequent flyer”
- Promotion of better teamwork and partnerships through consumer and clinician engagement.
Health system benefits
- Reduced presentations to EDs, and improved access to urgent care.
- Reduced unplanned readmissions and increased availability of resources for the community.
- Reduced acute healthcare costs and improved hospital performance.
Project status
Background
The VIP program seeks to identify and address the factors which can lead a person to repeatedly seek hospital care. It is widely accepted that a person’s health status is in part determined by factors beyond a person’s control. The social determinants of health, include elements such as access to healthcare, living conditions, availability of social supports, socioeconomic position, access to transport, and healthy food. Local and international evidence shows that these factors can lead to people accessing care in a hospital, when earlier intervention might have prevented them becoming ill. The situation can be impacted by an underlying mental health issue or disability which makes managing at home difficult, or they are socially isolated and lack support structures. Because general needs are not met in the community, such patients may seek hospital care frequently, representing to the ED multiple times.
Implementation
The VIP program, was piloted across three hospitals in the Hunter Region of New South Wales, Calvary Mater Newcastle, The Maitland Hospital, and Kurri Kurri District hospital. The program is based on the key elements of:
- Identifying our VIPs
- Alerting clinical teams to their arrival at the hospital
- Engaging with the person and their carers to understand their situation and the factors which have led them to seek hospital care
- Developing and implementing a plan of action to address those factors
- Maintaining a schedule of monitoring and support once they leave hospital.
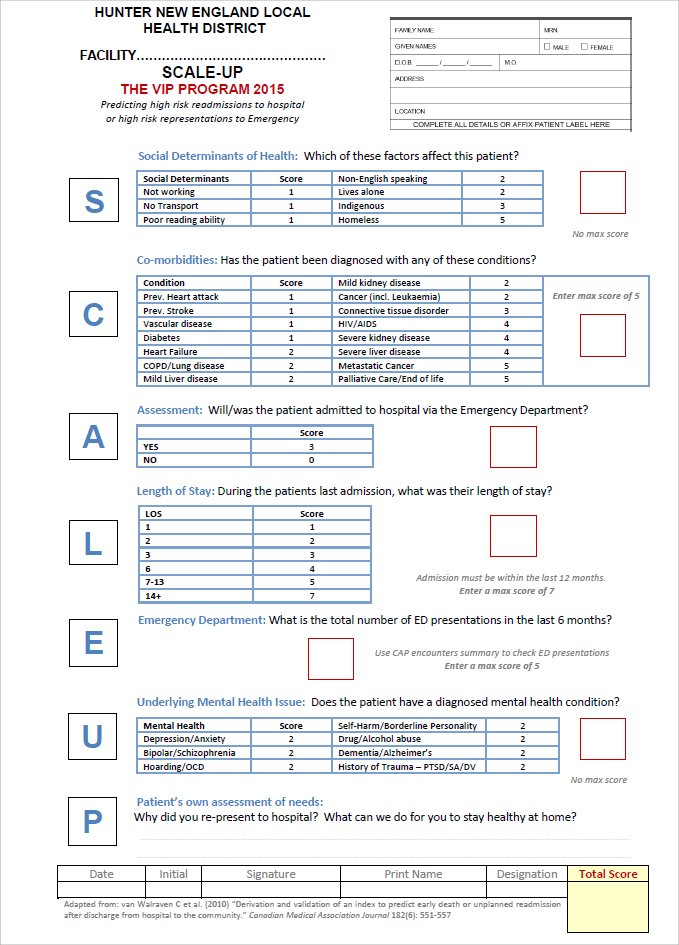
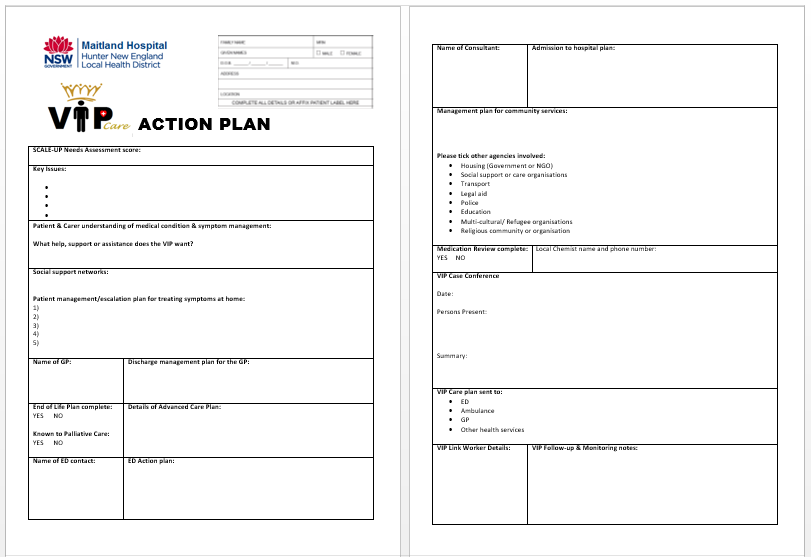
Our objectives have been to identify people at highest risk for re‐presentation to the ED or readmission to hospital and implementing personalised care plans that are seamlessly integrated across the acute and community setting. Our research has characterised potentially remediable psycho-socioeconomic risk factors for repeat ED representation and unplanned readmissions and enabled the development of the “SCALE‐UP” needs assessment tool (see Attachment 1). This tool identifies a person’s risk factors and enables clinicians to accurately identify medical and social care needs and implement an appropriate management plan.
Translation
- HNE‐LHD – Calvary Mater Newcastle, Maitland hospital, Cessnock hospital, Dungog hospital, John Hunter Hospital, Belmont hospitals, Mental health
- Nyngan Health Service, NSW
- Nepean hospital, NSW
- Port Macquarie hospital, NSW
- Central Coast LHD, NSW
- Caboolture Hospital Queensland
- Kalgoorlie Health WA
- Launceston City Mission collaborative, Tasmania
- Cabrini Hospital, Group Victoria
- Royal Melbourne Hospital group, Victoria
- Calvary hospitals, ACT & SA
- Orange and Bathurst hospitals, NSW
- Calvary Mater Newcastle
- The Maitland Hospital
- Kurri Kurri District Hospital
Key dates
- Project start: February 2015
Status
Sustained – The project has been implemented and is sustained in standard business.
Partnerships
The VIP program has consistently promoted better teamwork and partnerships through high levels of consumer and clinician engagement, peer support and increased staff capability for quality improvement. The use of redesign methodology has brought existing health roles together (including allied health, nursing, specialist medical staff and Ambulance for prehospital care) to tailor focused pathways for VIPs. Quarterly inter‐agency meetings involving over 29 health and social care stakeholders have continued to foster better integration across the local health system. Importantly the VIP program has continuing Executive support, and has been identified on the organisational, whole‐of‐health and winter planning strategies.
Results
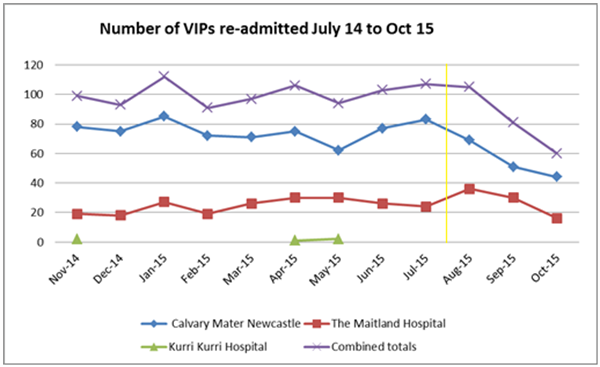
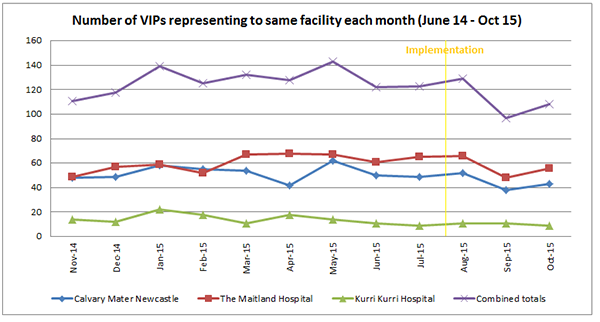
The initial results in 2015 showed that VIP unplanned readmissions reduced by 44% in the first three months. By March 2017 the program had achieved a further 21% average reduction across all three sites, equivalent to approximately 150 hospital admissions avoided. This progress has been sustained over the last 5 years; data in February 2019 showed that Calvary Mater alone had avoided approximately 450 hospital admissions since implementation, which is equivalent to a saving of 2250 bed days. As a dollar value this would equate to more than $1.57M in acute care costs. The VIP program has also delivered positive patient outcomes in relation to quality of care and hospital experience. VIPs reported that they are now strongly involved in decisions about their health, and had a clear point of contact to a care coordinator.
Further reading
- Boston University Medical Center. Project Re-Engineered Discharge (RED). Agency for Healthcare Research and Quality; 2010.
- Boutwell A, Rutherford P. Summary: STate Action on Avoidable Rehospitalizations (STAAR) Initiative. USA: Institute for Healthcare Improvement; 2009.
- Calvillo-King L et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. Journal of General Internal Medicine 2013; 28(2): 269-282.
- Chan FWK et al. Risk factors of hospitalization and readmission of patients with COPD in Hong Kong population: analysis of hospital admission records. BMC Health Services Research 2011; 11: 6.
- Coventry PA, Gemmell I, Todd CJ. Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: a cohort study. BMC Pulmonary Medicine 2011; 11(1): 49-58.
- Hu J et al. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Affairs 2014; 33(5): 778-785.
- Kansagara D et al. Risk prediction models for hospital readmission: a systematic review. Journal of the American Medical Association 2011; 306(15): 1688-98.
- Minmin M et al. Quality of life and its association with direct medical costs for COPD in urban China. Health & Quality of Life Outcomes 2015; 13(1): 1-6.
- Muenchberger H, Kendall E. Predictors of preventable hospitalization in chronic disease: priorities for change. Journal of Public Health Policy 2010; 31(2): 150-163.
- Osborn CY, Harrell F, Kripalani S. Determinants of health after hospital discharge: rationale and design of the Vanderbilt Inpatient Cohort Study (VICS). BMC Health Services Research 2014; 14(1): 1-20.
- Owens JM, Garbe RA. Effect of enhanced psychosocial assessment on readmission of patients with chronic obstructive pulmonary disease. Social Work in Health Care 2015; 54(3): 234-251.
- Purdy S. Tackling avoidable hospital admissions: improving or compromising quality? Quality in Primary Care 2012; 20(4): 243-244.
- Silow-Carroll S et al. Reducing Hospital Readmissions: lessons from top-performing hospitals. The Commonwealth Fund Synthesis Report; 2011.
- Society of Hospital Medicine. BOOSTing Care Transitions Resource Room. John A. Hartford Foundation Inc; 2008.
- Van Walraven C et al. Derivation and validation of an index to predict early death or unplanned readmission. Canadian Medical Association Journal 2010; 182(6): 551-557.
Contacts
Roslyn Barker
Patient Flow Manager
Hunter New England Local Health District
Phone: 0411 281 879
Roslyn.Barker1@health.nsw.gov.au