The Central Coast Local Health District (CCLHD) Oral Health Service is improving the provision of denture services. There will be a fairer and more efficient patient journey through the system, improved communication with patients, and clearer processes for staff. The waiting list for denture assessment will be reduced, and patients will be clinically assessed rather than rely solely on a telephone triage questionnaire.
View a poster from the Centre for Healthcare graduation, December 2018.
Aim
To improve access for eligible high priority denture patients to an assessment by decreasing median waiting time from 14 months to 3 months by July 2019.
Benefits
Patients
- Early access to clinical triage and treatment based on clinical need
- Improved integration of clinical care
- Reduced variation in access to denture services
- Improved understanding of the denture process
- Increased positive experience of their dental journey
Staff
- Increased knowledge and understanding regarding systems and processes
- Improved communication across the dental team
- Increased positive experience with provision of denture services
Healthcare system
- Efficient and consistent systems and processes
- Improved management of resources
- Increased productivity
- Reduced did-not-attend rates
- Improved patient throughput
- Reduced patient time in service
- Reduced negative feedback from patients and staff
Background
In Australia there is no Commonwealth scheme similar to Medicare that provides universal access to dental services. Adult patients are able to access the NSW public dental service if they hold a current Centrelink concession card. This patient cohort are generally the most disadvantaged and vulnerable members of the population.
In November 2017, over 2000 patients were waiting, following telephone triage, on the highest priority denture assessment waitlist at CCLHD. These patients were waiting a median of 14 months (11 months outside the NSW Health benchmark of 3 months). Patient complaints indicated poor experience with their journey to obtain a denture. In May 2018, the oral health staff reported only 35% positive experience with the denture pathway, and only 22% of staff reported that the current systems and processes supported their role.
All denture services at CCLHD are outsourced to private providers via the Oral Health Fee For Service Scheme. However there are inadequate and inconsistent processes in relation to quality control of dentures made which resulted in 9% of dentures being remade within three years (costing the service on average $1200 per patient).
Extended waiting times mean that conditions can often become acute or result in chronically poor oral health, with extended periods of discomfort or excessive pain. It may also add to the costs within the broader health system as dental treatment is sought from emergency departments and general medical practitioners.
Implementation
Issues
Four key issues were identified through data analysis and feedback from patients, staff and private providers.

- Variation in the way a patient gains access to denture services.
- Patient understanding and expectations regarding denture journey and the denture.
- Quality control of denture provision.
- Care coordination across the dental team.
Solutions
Five key solutions were identified to address these issues.
Solution 1: Agreed treatment plan

- Provides a written confirmation of treatment sequence, timing and likely outcome.
- Engages patients in treatment planning and managing expectations.
- A copy of the form is provided to patient to take for future reference.
- Addresses: Issues 2 and 4
- Status: Piloting (full implementation March 2019).
Solution 2: Local guideline for denture provision

- Provides a reference tool for clinicians.
- Standardises the criteria for denture provision, outlines different treatment options, and requirements for handover to private provider.
- Addresses: Issues 1 and 3
- Status: Drafting (full implementation March 2019).
Solution 3: Initial clinical assessment, currently known as ‘rapid assessment’

- Involves a ten minute appointment early in the patient journey to prioritise the patient’s clinical need and allocate them to the correct treatment waiting list.
- Addresses: Issue 1
- Status: Implementation and evaluation
Solution 4: Integrated consult

- One dentist working simultaneously with two hygienists (across two chairs) at the initial consultation to develop an integrated treatment plan.
- This solution will increase efficiency and communication, as traditionally patients are appointed separate consultation appointments with the dentist and the hygienist.
- Treatment planning will engage the patient, the dentist and the hygienist to ensure a better denture outcome and holistic care.
- Addresses: Issue 1 and 4
- Status: Planning (full implementation July 2019)
Solution 5: Private provider memorandum of understanding

- Improves communication and outlines mutual responsibilities and expectations between CCLHD and private providers.
- Addresses: Issue 3
- Status: Planning (full implementation April 2019)
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Key dates
- February 2018 – Start of project
- July 2019 – Plan to complete implementation of all solutions
- December 2019 – Plan to have all evaluations completed
Implementation sites
All dental clinics within CCLHD, with staggered implementation.
- Wyong Dental Clinic
- Gosford Dental Clinic
- Woy Woy Dental Clinic
Partnerships
Centre for Healthcare Redesign
Evaluation
Preliminary results
The following graph shows the median waiting time for the highest priority denture waiting list.
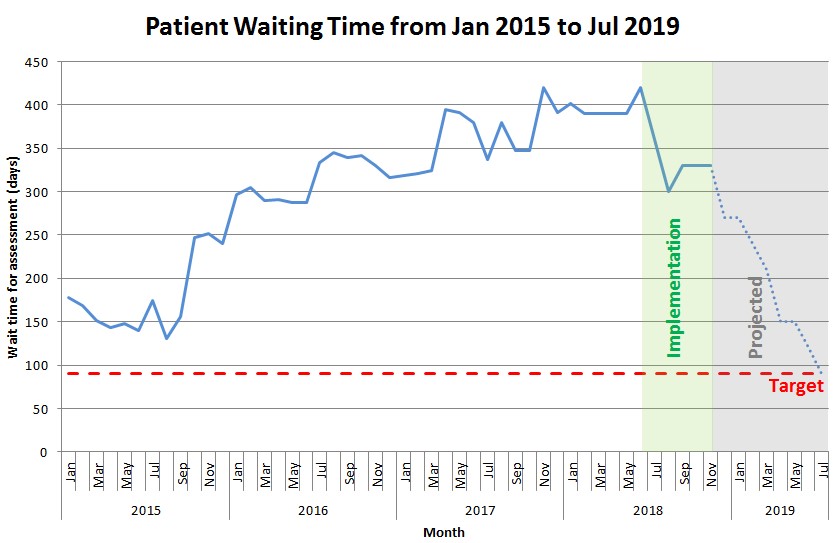
Over a four month period, 226 patients were seen over 18 sessions for an initial assessment (Solution 3), achieving progress towards Objective 1. We have calculated the capacity to assess the remaining patients outside of benchmark. We project they will be seen over the next six months, and will reach NSW Health benchmark by July 2019.
A complete evaluation will occur by December 2019.
- Median wait time for highest priority denture assessment
- Number of patients waiting over three months for highest priority denture assessment
- Staff experience survey
- Patient experience survey
- Denture remake rate (true impact of ‘remakes’ will not be able to be fully assessed for three years)
- IIMS notifications relating to dentures
Solution specific evaluation
Solution 1: Agreed treatment plan signed by clinician and patient
- Audit the proportion of high priority denture patients with an agreed treatment plan.
- Survey patients to assess involvement in health care decisions.
- Evaluation by December 2019.
Solution 2: Local guideline for denture provision
- Audit the proportion of staff who have read and signed-off on the guideline.
- Survey staff to assess the support of systems and processes.
- Audit patient files for application of guideline.
- Evaluation by December 2019.
Solution 3: Integrated consult
- Calculate proportion of high priority denture patients that are seen within an integrated consult appointment model.
- Calculate proportion of did-not-attend appointments.
- Evaluation by December 2019.
Solution 4: Initial clinical assessment
- Calculate number of patients waiting outside benchmark on highest priority denture assessment waitlist.
- Calculate reduction in highest priority denture assessment wait time.
- Evaluation by July 2019.
Solution 5: Private provider memorandum of understanding
- Memorandum of understanding published and signed by all private providers.
- Survey patients to assess denture satisfaction.
- Evaluation by October 2019.
Lessons learnt
- Allocate protected project time for the length of the project.
- Identify stakeholders, including patients, and engage them from the start of the project.
- Telling people ‘what to do’ is not enough to translate to action.
- Assign tasks, timelines and responsibilities to keep project on track - review at each meeting .
- Don’t assume you know what patients want.
- Develop multiple communication mediums and develop feedback loops.
- Allocate ‘breathing space’ for unexpected changes.
- Consider increased workload due to other departmental projects occurring simultaneously.
- Identify useful and informative diagnostic data.
- Scope creep is hard to avoid.
Contact
Leeann Mullen
Service Improvement and Quality Manager
Oral Health Service
Central Coast Local Health District
Phone: 02 4394 8312
leeann.mullen@health.nsw.gov.au