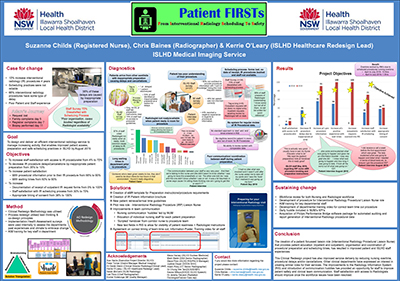
This project was a complete redesign of interventional radiology (IR) processes. This includes improving:
- scheduling practices
- protocolling practices
- patient experience
- patient information
- communication between team
- clinical handover.
View a poster from the Centre for Healthcare Redesign graduation, August 2019.
Aim
By August 2019, to design and deliver an efficient interventional radiology service to manage increasing activity and improved:
- patient access
- patient preparation
- safe scheduling of patients
- decreased waiting times in Illawarra Shoalhaven Local Health District (ISLHD).
Benefits
- Patients are prepared correctly for their interventional procedure therefore reducing delays and cancellations.
- Procedures are scheduled when radiologists are available during the day to reduce patient waiting times.
- Reduction in IR procedure wait times and cancellations will reduce patient stay in hospital.
Background
Despite a 10% increase in IR procedures in the last four years, procedure scheduling practices and organisation of patient preparation has not been updated.
Recent data on IR procedures and associated scheduling processes was captured across eight random sample days. This took place between December 2017 and July 2018. It showed that 66% of procedures have some type of delay. These delays include:
- inadequate patient preparation – 35%
- inadequate staffing and/or scheduling conflict – 23%
- a radiologist not being available – 15%
- other, not specified – 27%.
As an example, an incident also occurred where a patient’s imaging guided biopsy was delayed by 11 days, as the request was not scheduled. During this 11 day period, the patient’s daughter expressed concerns to the medical team regarding delays in her father’s treatment.
Currently in ISLHD the average length of stay in hospital is four days. This delay more than doubled the inpatient stay, which increases the cost of healthcare and potentially blocks a bed for two other patients.
Procedures often do not start on scheduled times, causing medical imaging nursing staff to be uncertain of daily workload, to miss allocated breaks and to work overtime (15.5hrs over a four month period at a cost of $1,113.51).
As one staff member stated: “Nothing has changed we just tack procedures on at the end of the day”. (Nurse, August 2018).
During the diagnostic phase, nine issues were identified that contributed to these delays and extended wait times.
People involved in this diagnostics and solution design process include:
- medical imaging staff
- other ISLHD nursing and medical staff
- patients.
Implementation
The following solutions have been implemented.
Interventional radiology procedure liaison nurse (pilot)
Implemented from 1 April 2019.
Steps
- Standard patient preparation notification and instructions for other ISLHD staff via electronic medical records template.
- Digital entry of paper outpatient request forms into the radiology information system.
- Outreach to ward patients in person and via phone to outpatients to improve communication and ensure correct preparation of patient.
- Improve the scheduling process to ensure a radiologist, staff and equipment available for each procedure.
- Update IR scheduler to contain radiologist meetings and reflect actual procedure times.
- Development of patient information booklet provided to patients during outreach
- Business case developed and supported by sponsors to make the role permanent.
New fields in radiology information system
Implemented on 10 June 2019.
Steps
- Improved communication between multidisciplinary team with 'Patient Ready Status' (prep commenced, prep completed, ready for room).
- Radiologist protocol IR procedures digitally. All staff can access information and accurately hand over relevant information and whether special equipment is required.
Work flow
Work flow pilot for inpatient pick up and outpatient presenting for procedures to reduce patient wait times in the department on April 10 2019.
Steps
- Agreed framework for inpatient pick up from ward 45 minutes prior to procedure.
- Agreed framework for outpatients to present 30 minutes prior to procedure.
Introduction of morning huddles
Implemented on 21 May 2019.
Steps
- Attended by nursing staff and modality seniors as able.
- Discuss work flow for the day and allocate nursing staff to procedures.
- Discuss any special equipment required.
- Staff have the ability to ask questions.
Introduction of structured handover
Implemented on 5 June 2019.
- Script developed and staff training in progress
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- July 2018 - Project start
- November 2018 - Diagnostics complete
- April 2019- Interventional radiology procedural liaison nurse pilot
- June 2019 - Evaluation of solutions
- November 2019 - Project completion date
Implementation sites
Medical imaging department, Wollongong Hospital. This provides all IR procedures for every hospital within the ISLHD area.
Partnerships
- NSW Agency for Clinical Innovation. Centre for Healthcare Redesign
- University of Tasmania
Results
Interventional radiology procedure liaison nurse (pilot)
Inpatient experience
Inpatient experience stories started on 12 July 2019, with positive feedback to date.
“Yes, she came and explained what was going to happen and gave me an information booklet. I was very glad she did, as I was awake for my procedure and I was warned not to worry about the noises, the loud clicks, during my biopsy. I knew what was going to happen and how long it was going to take. It took all the worry out of what was going on.” (Inpatient)
“Yes, she came and explained what to expect and gave me the information booklet. I wasn’t too worried about it, but I can see how doing that would reduce people’s anxiety.” (Inpatient)
Outpatient experiences
Stories started on 25 July 2019 with improvement recorded as follows.
- Auditing of outpatient request forms scanned shows improvement from 0% pre implementation to 82% post implementation (n=17 26.6.19-12.7.19)
New fields in radiology information system
Work flow pilot for inpatient pick up and outpatient presenting for procedures to reduce patient wait times in the department.
- Auditing of patient wait times in department started on 16 April 2019.
- Auditing of use of patient ready status started weekly from 23 July 2019.
- Ongoing plan, do, study, act (PDSA) cycles for improvement.
Introduction of morning huddles
- Observational audits done between Tuesday and Friday each week, starting on 4 June 2019.
- Daily huddle has become business as usual. Improved department communication and patient preparation allocation.
- Staff semi-structured interviews started in July 2019.
Feedback
“The benefits of the huddle are that everyone is involved…and we can voice any concerns, things that are working well. We get to know what is going on with the patient list for the day. It prompts us to different patient alerts e.g. if we have to make sure the patient had IDC (indwelling catheter) or has not received medication etc.”(Nurse)
Lessons learnt
- Change is hard!
- Projects do not succeed without strong effective sponsorship.
- Understanding your targets frame of reference is half the battle.
- Staff will readily embrace change when they see it has a positive effect on patient outcomes or service delivery.
- There is a massive difference between implementation and just installation. Coaching and positive reinforcement is essential for sustaining change.
- Ensure you double check who is on the email recipient list before hitting send.
Further reading
- Butler S. Prevention of Communication Failures in Radiology or Procedural/Interventional Settings. Journal of Radiology Nursing. 2018 Sep 1;37(3):145-6.
- MacDonald SL, Cowan IA, Floyd R, et al. Measuring and managing radiologist workload: application of lean and constraint theories and production planning principles to planning radiology services in a major tertiary hospital. Journal of medical imaging and radiation oncology. 2013 Oct;57(5):544-50.
- Waite S, Scott JM, Drexler I, et al. Communication errors in radiology–Pitfalls and how to avoid them. Clinical imaging. 2018 Sep 1;51:266-72.
- Zafar AM, Suri R, Nguyen TK, et al. Understanding Preprocedure Patient Flow in IR. Journal of Vascular and Interventional Radiology. 2016 Aug 1;27(8):1189-94.
Contacts
Suzanne Childs
Illawarra Shoalhaven Local Health District
suzanne.childs@health.nsw.gov.au
Chris Baines
Illawarra Shoalhaven Local Health District
Chris.Baines@health.nsw.gov.au