St Vincent’s Hospital Sydney is working to improve patient and staff safety, and the overall experience in the emergency department (ED). The focus is on eliminating extended lengths of stay in the ED. This will be achieved by implementing:
- an escalation process for patients who spend more than 12 hours in ED
- the use of patient care boards at each patient bedside across the hospital to better inform the patient of the planning around their discharge
- a real-time decision-tool to predict safe patient discharge from the ED.
View a poster from the Centre for Healthcare Redesign graduation, August 2019.
Aim
To improve patient and staff safety and experience in the ED to achieve zero patients who stay in ED for more than 24 hours. This would represent a reduction from 745 patients in 2017 to 2018, to zero patients by December 2019.
Benefits
Patients and families
The overarching benefit is an improvement in patient safety and experience when they present to the ED.
- A patient presenting to St Vincent’s Hospital Sydney will not have an extended stay of more than 24 hours in the ED.1,2
- If in a ward bed at night, the patient will not be subjected to noise due to 24/7 ED activity, nor will the patient suffer disorientation because they do not know whether it is day or night.3,4
- As a result of the decreased length of stay in the ED, the patient will have a reduced chance of developing delirium and subsequently suffering a fall.3,4
- This decreased length of stay also helps to avoid the scenario of a patient’s discharge date being later than their expected discharge date, which in turn has a knock-on effect. It means the ward bed is unable to be used by an admitted patient sitting in the ED. Or a patient waiting on an elective surgical procedure may have that procedure cancelled due to the lack of an inpatient bed.5,6
- Timely access will be provided to medical and nursing care, for acutely unwell patients presenting to the ED at St Vincent’s Hospital Sydney.5,6
- A reduction in ED overcrowding, which is known to be a predictor of delays in timely access to treatment, such as the prescribing and administration of antibiotics and/or analgesia.5-9
St Vincent’s Hospital Sydney and St Vincent’s Health Australia
The overarching benefit is a decreased cost of care.
- If a patient receives the right care, in the right place, there is a subsequent decrease in cost. This is because the patient receives care in the appropriate setting. The cost of keeping a patient in ED is twice as much compared to managing a patient in a ward bed. This is owing to differences in staffing levels, and often, the complexity of care.10,11
- This contributes to us achieving the St Vincent’s Health Australia’s mission and values of ‘leading through research driven, excellent and compassionate health and aged care, with justice and integrity.’2
St Vincent’s Hospital Sydney ED staff
The overarching benefit is improved staff safety and staff experience.
- An improved working environment for ED clinical and non-clinical staff, which will result in staff being less likely to report frustration at continually having to find somewhere to see, assess and initiate treatment for a patient who presents acutely unwell to the ED.5,8
St Vincent’s Hospital Sydney – ward based staff
The overarching benefit is reduced frustration and a more supported experience.
- Inpatient unit medical and nursing staff will report less frustration if the patient is admitted in a timely manner to a ward bed – the patient will receive the specialist care they require from nurses and doctors educated in providing that specialist care, at St Vincent’s Hospital, Sydney.5,8
For the NSW healthcare system including the Ambulance Service of NSW
The overarching benefit is improved access to care.
- Overall sustained improvement in the Transfer of Care of patients presenting by ambulance and then transferred to the care of ED staff. This is in support of NSW Ministry of Health key performance indicators ≥ 90%).12
- Ambulances will be where they are needed , which is in the community as first responders to patients who require emergency medical care.
- Overall sustained improvement of Emergency Treatment Performance when a patient presents to the ED. This is in support of NSW Ministry of Health target ≥ 81%.13
- Patients will receive timely medical and nursing care when presenting to the ED at St Vincent’s Hospital Sydney.5-9
Background
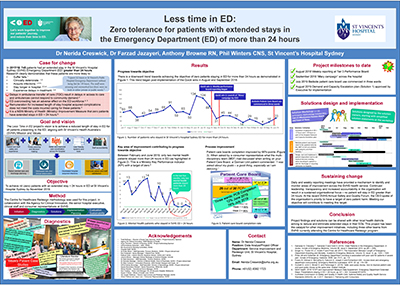
In the 2017/2018 financial year, 745 patients stayed in St Vincent’s Hospital Sydney’s ED for over 24 hours, when both the NSW Ministry of Health, and St Vincent’s Health Australia’s target is zero.1,2 Given the link between length of stay in the ED and poor clinical outcomes, St Vincent’s Hospital Sydney is working to improve the overall experience of being a patient, or a staff member working in the ED, while also optimising both patient and staff safety, with a focus on reducing patients’ ED length of stay, by December 2019.3-9 Ultimately, the overall objective is to achieve zero patients with an extended stay greater than 24 hours in the ED at St Vincent’s Hospital Sydney, by December 2019.
When patients presenting to ED receive the right treatment, within the right time frame and in the right place, whether admitted to a ward bed or treated and discharged from the ED, they are less likely to have an adverse outcome.3-5 Moreover, if an admitted patient is occupying an ED bed, this has a knock-on effect restricting access for people presenting to the ED acutely unwell.5-9 ED clinicians also report frustration when unable to find a safe clinical space to assess the patient and to commence safe and timely emergency care.5,8
Implementation
Quick win 1. Weekly report at tier 3 performance board
- Since August 2018, data of patients with an extended stay in the ED greater than 24 hours has been presented by the project team in conjunction with the weekly hospital access and demand report. Evidence of success is shown by the decreasing number of patients staying in the ED greater than 24 hours.
- Fortnightly root cause analysis of the patient with the longest length of stay in the ED over the last 14 days (n = 15).
- Ownership and increased accountability by stream directors, heads of medical specialities and departmental managers at tier 3, for patients who have an extended stay greater than 24 hours in the ED.
Quick win 2. ‘Mary Campaign’ across the hospital
- Poster campaign launch by email from the hospital chief executive officer to all staff highlighting the importance of patients moving through the ED in a timely manner for their safety, and with a focus that staff remember that patients have a name and are not simply a medical record number or the ‘hip in bed 10’.
- Implemented by project team in consultation with the communications department and the project’s executive sponsor.
- Evaluated by survey of ED staff following the campaign: 84% (n=36) agreed or strongly agreed that patients who have a length of stay of stay in the ED greater than eight hours are at risk of poor outcomes.
Three areas of focus
Three areas of change or focus are required if this project is to achieve zero patients with an extended stay greater than 24 hours, by December 2019.
Solution 1. Implementation of a demand escalation plan
What happens when a patient in the ED is waiting for more than 12 hours for a ward bed? Or is waiting to leave the ED? A demand escalation plan is required to clearly outline hospital-wide actions to be taken when a patient is approaching 12 and 24 hours in the ED.
Implementation includes
- Meetings began in April 2019 between patient flow, ED medical and nursing staff and stream managers to identify the triggers and actions they currently undertake to escalate and respond to a surge in activity, across their clinical areas.
- The patient flow manager, whole of health lead and the ED worked together to draft an escalation matrix and task cards.
- Revision and refinement of escalation plan was conducted in May and June 2019.
- The plan was approved by the St Vincent’s Hospital Sydney senior leadership team in July 2019, as part of the larger Demand and Capacity Escalation Plan.
- Education sessions were scheduled for delivery across the hospital in August 2019.
- Ongoing evaluation continues into the Demand and Capacity Escalation Plan between August to December 2019
- Launch of finalised Demand and Capacity Escalation Plan is scheduled for February 2020.
Solution 2. Use of the bedside patient care board
- This will help patients and their families achieve their care goals and have an awareness of the planning for their expected discharge date. Patient care boards need to be updated daily, in full consultation with patients and their family, either by the multidisciplinary team or the nurse allocated to that patient.14
- The nursing staff are to manage the patient care boards. Completion of patient care boards will be randomly measured weekly and will be reported to Tier 1 and Tier 2 weekly meetings.14
Implementation includes
February 2019
- Meeting between the reinforcing sponsor, solution two consultant and whole of health patient flow clinical lead to present the use of the patient care boards.
March 2019
- Meeting with ‘Intentional Rounding’ project lead, to gain feedback and to check for any competing issues with the patient care boards.
- Meeting with ‘Nurse Unit Manger’s Resource’ project lead, to discuss inclusion of the weekly patient care boards audit and reporting pathway.
- Correspondence with suppliers about the design and purchase of consumables, such as white board marker pens and erasers.
- Meeting with the Sacred Heart Rehabilitation Unit, the Palliative Care ward and the Gorman Unit were identified as being keen to introduce patient care boards after discussion late March 2019.
April 2019
- Meeting with St Vincent’s Hospital Sydney consumer representatives to allow feedback in the design and implementation.
- Meetings across March and April with the reinforcing sponsor to provide patient care board updates and to discuss the current ‘Bedside Handover Project’ and also to cross check with project heat map.
May 2019
- Meeting with the communications director at St Vincent’s Hospital Sydney, to discuss the design of a promotional campaign for Patient Care Boards’ implementation phase.
June 2019
- Additional patient care boards for Sacred Heart Rehabilitation Unit, the Palliative Care ward and the Gorman Unit installed.
- White board marker pens/eraser were supplied for each patient care board.
- Meeting with executive sponsor, reinforcing sponsor, clinical lead - Intentional Rounding, Work Safe consultant to:
- report on ward audit of patient care board placement with Work Safety.
- review patient care board adhesive window signage quote from Imagination Graphics
- decide that patient care boards will be phased in under Intentional Rounding.
Solution 3. A real-time decision-making tool
- To design, test and implement a simple user friendly decision tool or scoring system to stratify a patient’s early discharge risk, allowing ED doctors to identify if a patient is safe for early discharge from the ED.
- This will stratify a patient’s early discharge risk before the decision to admit is made by ED doctors, potentially reducing the patient length of stay in the ED at St Vincent’s Hospital Sydney.15,16
Implementation includes
- February 2019: Meetings between project team began with solution owners.
- April 2019: Further collection and analysis of not admitted data and a literature review write up as part of evidence diffusion strategy.
- May 2019: Email correspondence with the Glasgow Royal Infirmary, in the United Kingdom, and Royal Prince Alfred Hospital Sydney, after a literature review revealed that other jurisdictions are looking at methodologies to predict patient disposition from point of triage to improve patient flow.
- June 2019: Further meeting with executive sponsor, clinical leads and solution owners.
Phases
- Phase 1: Minutes, literature review and relevant journal articles sent to key stakeholders from executive sponsor.
- Phase 2: Meetings scheduled with gerontology and thoracic medicine to discuss pilot phase of patient disposition prediction tool.
- Phase 3: Solution 3 consultation phase – confirm design and testing of tool.
- Phase 4: Testing phase with small cohort of patients from gerontology or thoracic medicine.
- Phase 5: Evaluation of phase four – scheduled for September 2019.
- Phase 6: Implementation phase five across all specialties – scheduled for September/October 2019.
- Phase 7: Evaluation of phase five looking at Solution 3 sustainability – October 2019.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- Project planning: March to May 2018
- Project initiation: May to September 2018
- Diagnostics: May 2018 to November 2018
- Quick win 1 implementation (Report at weekly Tier 3 Performance Board): August 2018
- Quick win 2 implementation (“Mary” campaign launched by email from the Chief Executive Officer of St Vincent’s Sydney): October 2018
- Solutions design: December to January 2019
- Implementation planning: February to March 2019
- Implementation of Solution 1: August 2019
- Implementation of Solution 2 (Patient care boards) installation: April 2019
- Design and piloting of Solution 2 measurement system: May 2019
- Implementation of Solution 2 Phase 1: July 2019
- Evaluation of Solution 2 Phase 1: scheduled for August 2019
- Implementation of Solution 2 Phase 2: scheduled for August 2019
- Review of Solution 1: December to January 2019
- Implementation of finalised Solution 1: February 2019
- Ongoing evaluation of all solutions: scheduled for July 2019 to July 2020
- End date: July 2020
Implementation sites
- Solution 1: St Vincent’s Hospital Sydney, Darlinghurst Campus: ED, all inpatient units.
- Solution 2: St Vincent’s Hospital Sydney, Darlinghurst Campus: Phase 1
- in sub-acute areas: Rehabilitation and palliative care, and
- acute areas - the Gorman Unit (substance abuse detox unit).14
- Solution 3: Phase 2 - Darlinghurst Campus: gerontology and thoracic medicine departments.15,16
Partnerships
- Acute Medicine Unit, Glasgow Royal Infirmary, Glasgow, United Kingdom.
- Centre for Healthcare Redesign
- Gosford Hospital, Central Coast Local Health District.
- Royal Prince Alfred Hospital, Sydney - ED.
- St Vincent’s Hospital Melbourne, ED.
- University of Tasmania.
Results
- The number of patients staying in the ED for more than 24 hours has reduced by 36%. This is from 745 in 2017/2018 to 480 in 2018/2019.
- The number of mental health patients staying in the ED more than 24 hours has reduced by 45%. This is from 88 in 2017/2018 to 480 in 2018/2019 (a Ministry of Health timeliness and accessibility key performance indicator).
- These results have been driven by the implementation of the two quick wins.
- Preliminary results for the use of bedside patient care boards in two wards has led to a 66% point improvement in patient care board completion, with a baseline completion rate of 12% in June 2019 increasing to a 78% completion rate in July 2019.
Lessons learnt
- Follow the method – let the method, such as the Centre for Healthcare Redesign Method, guide you through the process. This will ensure that the root causes are identified during the diagnostics phase and that the problem will be addressed with appropriate solutions.
- Good sponsorship is key to driving change in the organisation.
- Ensure all stakeholders are kept informed throughout the project phases – it is easy to forget about some of them when working away at the project deliverables.
- Be flexible when resistance impacts on the implementation phase.
References
- NSW Health Service Agreement: 2018 – 2019 Improvement KPIs. Strategy 2 IMs: Integrate systems to deliver truly connected care: KSA201- ED extended stays: Presentations staying > 24 hours (Target = Zero), pp 321 – 322. Accessed 8/1/2019
- St Vincent’s Health Australia - enVision2025. Our Strategy 2025. www.svha.org.au. Accessed 8/1/2019
- Samaras N, Chevaley T, Samaras D and Gold G. Older Patients in the Emergency department: A review. Annals Emergency Medicine. 2010 Sep; 56 (3): 261-9. https://www.ncbi.nlm.nih.gov/pubmed/20619500. Accessed 8/1/2019
- Singer A J, Thode HC Jr, Vicello P and Pines JM. The Association Between Length of Emergency department Boarding and Mortality. Academic Emergency Medicine, 2011. Volume 18, issue 12, pp. 1324 – 1329. https://www.ncbi.nlm.nih.gov/pubmed/22168198. Accessed 8/1/2019
- Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity. Annals of Emergency Medicine. 2002, Volume 39, Issue 4, pp. 430 – 432, viewed 26 September 2018. https://www.ncbi.nlm.nih.gov/pubmed/11919530. Accessed 8/1/2019.
- Forero, R, Hillman K, McCarthy S, Fatovich D, Joseph, A and Richardson, DW. Access block and emergency department overcrowding. Emergency Medicine Australasia. 2010. 22, pp. 119 -135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3219412. Accessed 8/1/2019.
- Pines JM and Hollander, JE. Emergency department crowding is associated with poor care for patients with severe pain. Annals Emergency Medicine. 2008. Jan; 51(1), pp. 1-5, viewed 25 September, 2018. https://www.ncbi.nlm.nih.gov/pubmed/17913299
- Derlet RW and Richard JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Annals of Emergency Medicine. 2000 Jan; 35(1):63-8. https://www.ncbi.nlm.nih.gov/pubmed/10613941. Accessed 8/1/2019.
- Fee C, Webber EJ, Maak CA, Bacchetti P. Effect of Emergency department Crowding on Time to Antibiotics in Patients admitted With Community-Acquired Pneumonia. Annals of Emergency Medicine. Nov. 2007. Vol 50(5): 501 – 509. https://www.doi:org/10 1016/j.annemergmed.2007.08.003. Accessed 8/1/2019
- Schreyer K E and Martin R. The Economics of and Emergency Admission Holding Unit. West J. Emergency Med. June 2017: 18(4): 553 – 588. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5468058. Accessed 1/4/2019
- Independent Hospital Pricing Authority. National hospital cost data collection. Australian Hospitals Cost Report. 2015-16. Round 20. https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-public-hospitals-cost-report. Accessed 1/4/2019
- NSW Health Service Agreement: 2018 – 2019 Improvement KPIs: Strategy 2 KPI: Provide World Class Clinical Care where patient safety is first: KSA102 - ETP: total time in Ed < 4 hours (%) (Target = greater than or equal to 81%).
- Australian Commission on Safety and Quality in Health Care: National Safety & Quality Health Standards (NSQHS). Standard 2 Partnering with Consumers Standard; Standard 5 Comprehensive Care Standard; Standard 6 Communicating for Safety Standard. https://www.nationalstandards.safetyandquality.gov.au/. Accessed 8/1/2019.
- Dinh MM, Berendsen Russell S, Bein K J, Rogers K, Muscatello D, Paoloni R, Hayman J, Chalkey DR and Ivers R. 2016. The Sydney Triage to Admission Risk tool (START) to predict Emergency Department Disposition: A derivation and internal validation study using retrospective state-wide data from New South Wales, Australia. Emergency Medicine pp 16:46. doi 10.1186/s12873-016-0111-4
- Cameron A, Rodgers K, Ireland A, Jamdar R and McKay GA. 2015. A simple tool to predict admission at the time of triage. Emerg Med J; 32:174 – 179. doi: 10.1136/emermed-2013-203200
Contacts
Dr Nerida Creswick
Data Analyst/Project Officer – Project Lead
Service Improvement and Redesign Unit
St Vincent’s Hospital, Sydney
Phone: +61(0)2 8382 1723
nerida.creswick@svha.org.au
Dr Farzad Jazayeri
ED staff specialist – Clinical Lead
Emergency department
St Vincent’s Hospital, Sydney
Phone: +61(0)2 8382 2473
farzad.jazayeri@svha.org.au
Anthony Browne
Registered Nurse
Emergency department
St Vincent’s Hospital, Sydney
Phone: +61(0)2 8382 2473
anthony.browne@svha.org.au
Phil Winters
Clinical Nurse Specialist
Patient Flow Navigator – Wards 8 North and 8 South
St Vincent’s Hospital, Sydney
Phone: +61(0)2 8382 1111 (Switchboard)
philip.winters@svha.org.au