This project aims to improve the identification of clients who may be violent or aggressive towards St Vincent’s Hospital Network staff working in the community.
View a poster from the Centre for Healthcare Redesign graduation, December 2018.
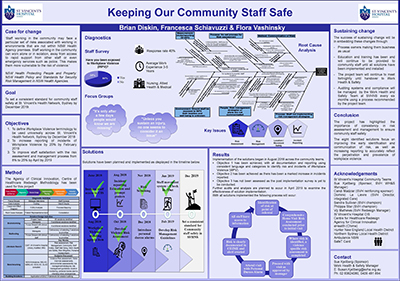
Aim
To set a consistent standard for community staff safety for the St Vincent’s Hospital Network, Sydney by December 2019.
Benefits
- Reduced emergency department and clinic presentations due to adequate care being provided in the community.
- Reduced sick leave taken by community staff resulting from incidents of violence and aggression.
- Reduced turnover of community staff associated with the consequences of incidents of violence and aggression.
- Improved community staff satisfaction with the violence and aggression risk assessment and management process.
- The clients seen in the community are appropriate and staff safety is ensured throughout service provision.
Background
Workplace violence directly affects health provision and can lead to a reduced quality of care provided to patients. Work environments which focus on and support the health, safety, and wellbeing of staff, help to create improved patient and staff outcomes.
At St Vincent’s Health Network (SVHN), some community teams have developed local risk assessment and management strategies. However, the process to identify individuals at high risk of violence and aggression is inconsistent across the network, one identified reason being that different teams use different clinical health information systems. Furthermore, staff understanding of what constitutes violence and aggression is inadequate with each clinician’s threshold for violence varying greatly.
Some staff have adopted the view that violence and aggression is an accepted part of the job. Research shows that when staff accept workplace violence to be part of the job they are more likely to become victims themselves.1
The project team conducted a controlled survey of community staff which sought to gauge staff views on workplace violence and aggression. The results indicated that:
- 8% of staff find the current risk assessment process effective
- 69% rely on tick-box risk assessment
- 18% of respondents have questioned their position in the community due to exposure to workplace violence
- 25% have experienced sexual aggression
- 16.5% have experienced physical aggression
- 61% ‘never’, ‘rarely’ or ‘sometimes’ complete Riskman (incident report) following an incident of violence or aggression
- 65% of staff felt ill-prepared to manage a violent incident
- 16% of staff have used leave due to the stress associated with workplace violence
- 19% felt that exposure to workplace violence has affected their personal life
- 42% perceive workplace violence to be part of the job.
There are ongoing financial and non-financial costs associated with violence and aggression in the workplace that can have a significant impact on the team involved in patient care. At SVHN the identified financial cost of a staff member seriously assaulted in the community is likely to be no less than $100,000. This includes medical care, associated costs of staffing, human resource involvement, work cover claims, and lost time injuries. Other negative impacts include organizational reputation, and the psychological and physical well-being of the staff member and their respective teams, including motivation and morale.
Implementation
In order to identify the need for the project to be undertaken, an initial staff survey was conducted to understand the current exposure and perception of violence and aggression towards staff working in the community. The results were inconsistent with data from Riskman (incident reporting system) and further exploration regarding the prevalence of workplace violence was required.
A project plan was developed outlining the scope, stakeholders, goals and objectives of the project. Through the diagnostics and solution design phases of the project a number of techniques were used to identify the key issues and develop solutions for the community services. These included:
- one-on-one interviews with community team managers
- focus groups with community team clinicians
- an anonymous staff survey of all clinicians working in the community
- one-on-one consultation with consumer representatives
- root cause analysis of identified issues by project team
- steering committee meetings for feedback and approval on solutions
- multi-voting to identified desired solutions from community clinicians
- workshops and in-services for implementation of identified solutions.
Following the extensive research and design stage, the following solutions were recommended.
- Develop violence risk assessment for use across community teams where it is not current practice.
- Provide unrestricted access across St. Vincent’s clinical information system (CHIME), to ensure staff can obtain collateral from information gathered by all services and disciplines.
- Develop a universal and reliable system to monitor staff movements and whereabouts.
- Introduce personal duress alarms for community staff.
- Develop a risk management process and guidelines.
- Provide risk screening on all referral, discharge, and transfer of care documentation.
- Workplace violence to be a standing agenda item at all staff meetings.
- Education on incident reporting and prompt posters.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
February 2018 – February 2019
Implementation sites
- St Vincent’s Hospital, Darlinghurst Community Teams
- Community Mental Health
- Homeless Health Service
- Flexicare Nursing
- Flexicare Allied Health
- Transitional Aged Care Program (TACP)
- Hospital in the Home (HITH)
- Chronic Care Initiatives
- Heart Failure Service
- Community Palliative Care
- Older People’s Mental Health Service
Partnerships
- Centre for Healthcare Redesign
- Agency for Clinical Innovation
- eHealth (Chime)
- Hunter New England Local Health District
- Northern Sydney Local Health District
- Ambulance NSW
- SafeT Card
Evaluation
The following evaluation processes will be executed following implementation to measure the effectiveness, sustainability, and staff use of the proposed solutions.
- Repeat staff survey.
- Audit compliance with risk assessment tools.
- Audit team meeting minutes.
- Including recommendations in St Vincent’s Hospital Home Visiting Policy.
- Handover to work health and safety team for ongoing auditing and monitoring of solutions.
Lessons learnt
- Take time with the diagnostics to really understand the issue
- Don’t assume what the issues are, let the issues be identified through discussion with key stakeholders
- Secure reinforcing sponsor support
- Engage clinicians throughout the entire process
- Use your champions to help mitigate issues with clinicians
- Expect resistance with implementation
References
- Trinkoff AM, Geiger-Brown JM, Caruso CC, et al. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville: Agency for Health Care Research and Quality; 2008.
Contacts
Brian Diskin
NUM Outpatients Department
St Vincent’s Hospital, Sydney
Phone: 02 8382 3116
James.diskin@svha.org.au
Francesca Schiavuzzi
Community Occupational Therapist
St Vincent’s Hospital, Sydney
Phone: 02 8382 1450
Francesca.schiavuzzi@svha.org.au
Flora Vashinsky
Psychologist
Community Mental Health Services
St Vincent’s Hospital, Sydney
Phone: 02 8382 1300
flora.vashinsky@svha.org.au