Southern NSW Local Health District (SNSWLHD) Drug and Alcohol (D&A) services are aiming to improve the client experiences of D&A service provision with a focus on timely access, evidence-based treatment and pathways to ongoing care and support in the community. The project is implementing a number of solutions to improve triaging of referrals, standardise treatment pathways and models for collaborative, step-down care through partnerships with general practitioners (GPs) and non-government organisations (NGOs). There is a particular emphasis on ensuring that priority populations, such as pregnant women and Aboriginal clients, receive care when they need it.
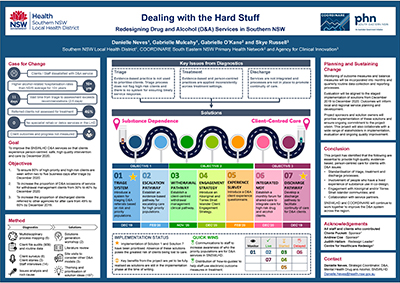
View a poster from the Centre for Healthcare Redesign graduation, August 2019.
Aim
This project aims to improve the SNSWLHD D&A services so that clients experience person-centred, safe, high quality intervention and care by:
- increasing the proportion of high priority and high risk clients who are seen within two to five business days after triage to 80% by December 2020
- increasing the proportion of acute D&A service consultations to clients detoxifying from 30% to 40% of occasions of service by December 2019
- increasing the proportion of discharged clients referred to other agencies for after care from 49% to 60% by December 2019.
Benefits
The project has already improved relationships between key stakeholders that include mental health drug and alcohol (MHDA) staff, emergency department (ED) staff and general ward staff, GPs and NGOs. Other benefits will include improved client experiences of the service demonstrated in reported experience measure questionnaires and improved continuity of care using streamlined discharge pathways.
In developing a community-led, co-design group to develop a strategy for Aboriginal and/or Torres Strait Islander engagement, the service will ensure clients receive a culturally appropriate D&A service.
Background
SNSWLHD covers an area of 44,534 square kilometres. The population is 202,000, of which 3.5% identify as Aboriginal.
The region is serviced by only 15 full-time equivalent D&A staff, and there are no inpatient D&A rehabilitation services available.
SNSWLHD D&A services are under stress, with clients, clinicians and managers reporting dissatisfaction with the current system. Diagnostic data from this project indicates that the median time from triage to assessment for the period June 1 2018 to August 31 2018 was 11 days. Clinical reviews and root cause analyses have highlighted clinical management issues, including limited communication between specialist D&A services and other care providers. This indicates a deficit in coordinated care for D&A clients.
Data from 2017 supports these findings, which indicated that only eight clients out of 1143 were referred to their GPs at discharge from D&A services.1 It is well documented that a lack of service integration results in repeated acute presentations to D&A services.2
Implementation
This project involves the implementation of seven solutions. Implementation of these solutions will be staggered over two years, as there are interdependencies between solutions.
The progress on implementation to date is detailed below.
- Introduce a triage system within SNSWLHD MHDA Triage and Emergency Care Support to identify risk for D&A clients and recommend timeframes for treatment. This will involve the introduction of an evidence-based D&A triage referral tool. At triage, clients will be routinely screened for pregnancy, recent incarceration, comorbid mental health issues and other psychosocial risk factors to ensure care is targeted to client priority and need.
- Develop an evidence-based pathway for escalating care for high priority populations. This is being designed and will be implemented after the triage process is established.
- Establish a client-centered withdrawal management clinical pathway, which will be co-designed with consumers and based on the evidence-based guidelines.
- Introduce an Aboriginal and Torres Strait Islander client engagement strategy for D&A services. An Aboriginal cultural competence training package has been designed and implementation began in August 2019.
- Introduce a D&A client experience questionnaire. Staff and clients are in the early stages of developing this tool and are collaborating, using co-design method.
- Establish a cross-service, multidisciplinary forum that facilitates interagency drug and alcohol clinical review and clinical management across service settings.
- Develop a discharge pathway for D&A clients, who require stepped-down or ongoing care. This will be designed in collaboration with GPs to support the transfer of care from specialist D&A services.
Status
Implementation – The initiative is ready for implementation, is currently being implemented, piloted or tested.
Dates
- Initiation: June 2018 - August 2018
- Diagnostics: August 2018 - January 2019
- Solutions: January 2019 - March 2019
- Implementation: April 2019 - December 2020
- Evaluation: Staggered from December 2019 to January 2021
Implementation sites
As this is a district-wide project, staggered implementation of the solutions will occur across five community MHDA sites.
Partnerships
The project is a partnership between SNSWLHD MHDA and the Primary Health Network, COORDINARE. Support by an ACI team member was available until the end of August 2019. Implementation of solutions will be dependent on strong relationships between Community D&A services, MH inpatient and generalist, inpatient settings.
Evaluation
The plan for evaluation is outlined below.
- Monitor outcomes and quality of all D&A triage referrals.
- Measure LHD acute withdrawal management activities.
- Monitor the percentage of referrals to external services and establish a feedback loop.
- Monitor the time taken from triage to assessment (11 days median, 12 days average at start of implementation) with the aim of achieving a 2-5 day median time from triage to assessment at the conclusion of project implementation.
- Measure the number of clinicians receiving cultural competence training, collect participant evaluations about training received and levels of confidence in providing culturally competent practice.
- Monitor and collate patient experience data collected through patient experience measures.
- Evaluation will be aligned to the staged implementation of solutions from December 2019 to December 2020.
Lessons learnt
- Although the application for ethics approval was lodged early, projects seeking publication should have ethics approval finalised from the outset, as delays in all stages of clinical redesign can result from delays in ethics approval.
- Implementing a project in a rural area requires innovative and varied approaches to ensure stakeholders are effectively engaged. Tackling the tyranny of distance required commitment to communicating with people face to face, where possible. We also used technology proactively to connect as a team and to connect with the service (e.g. video-conference and skype).
- When setting up a project team involving internal and external members, a cross-agency agreement should precede establishment of the project team. Where there is more than one sponsor, the complementary roles of sponsors from different agencies will need to be explored and articulated.
- When setting up a project team involving internal and external members, sourcing information technology platforms that meet NSW Health data security requirements may present logistical challenges and should be resolved at the project outset.
- Develop sensitive and diverse ways of collecting client input with marginalised, stigmatised populations. Do not rely on one method of collecting client data. Consider surveys, focus groups, interviews and ad-hoc consultations.
- Team members and project team leaders need to be flexible in balancing roles and responsibilities and the demands of task completion with the changing needs of the project.
- Data gaps need to be identified early otherwise the burden of manual data collection on the team may be considerable.
- Developing a clinical redesign project in a changing environment (for example, ongoing revisions to clinical service standards, changes in the type and number of non-government organisations operating in the district), requires a flexible, positive and responsive approach to clinical redesign. Using tools to assess organisational stress and planning accordingly as early as possible can help project teams in planning realistic time-frames, when there are multiple changes impacting on service operations.
- Identifying the role of the reinforcing sponsors and providing appropriate training and support is a significant step in ensuring project success. In our rural LHD, this involved multiple methods of communication, including formal and informal meetings, both face to face and using other technologies.
References
- SNSWLHD Mental Health Drug and Alcohol (MHDA) Performance Data. [Unpublished internal document]
- Australian Institute of Health and Welfare. Alcohol and other drug treatment services in Australia 2011-12. Drug treatment series 21. Cat. no. HSE139. Canberra: AIHW; 2013.
Contact
Danielle Neves
Strategic Co-ordinator, Drug and Alcohol
Mental Health Drug and Alcohol
Southern NSW Local Health District
Phone: 0436 680 581
Danielle.Neves@health.nsw.gov.au