The Breathe Easy project aims to eliminate varying treatment outcomes and clinical uncertainty for patients with exacerbation of chronic obstructive pulmonary disease (COPD), admitted to South East Regional Hospital (SERH) in Bega. This will be achieved by adhering to the Thoracic Society of Australian and New Zealand (TSANZ) guidelines that promote safe patient outcomes and patient engagement.1
View a poster from the Centre for Healthcare Redesign graduation, December 2018
Aim
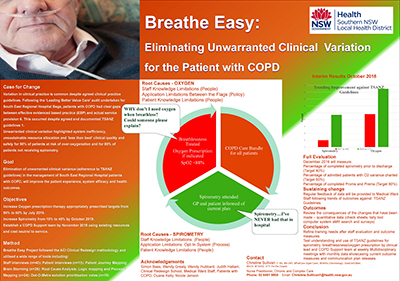
- Increase oxygen prescription therapy appropriately prescribed targets from 50% to 60% by July 2019.
- Increase spirometry from 10% to 40% by October 2019.
- Establish a COPD support team by November 2019 using existing resources and cost neutral to service.
Benefits
- Improved patient experience and health outcomes.
- Seamless integration of care for COPD patients.
- A reduction in hospital admissions and bed days for SERH.
- Improved communication between medical, nursing and allied health teams.
Background
Variation in clinical practice is common, despite the existence of agreed clinical practice guidelines.2-4 While no standardised definition quantifies clinical variation, the patient with ‘similar diagnoses, prognoses and demographic status who receives different levels of care depending on when, where and by whom they are treated’ will be the essential understanding.5
Audit results for identified admitted patients with COPD at SERH (n=40) showed clear gaps between effective evidenced based practice and actual service provision.6 This occurred despite agreed and documented TSANZ guidelines.1
Unwarranted clinical variation highlighted system inefficiency, unsustainable resource allocation and ‘less than best’ clinical quality and safety for 50% of patients at risk of over-oxygenation and for 80% of patients not receiving spirometry. It was hypothesised that elimination of unwarranted clinical variance (adherence to TSANZ guidelines) in the management of SERH Bega patients with COPD will improve the patient experience, system efficacy and health outcomes.
Implementation
Pilot planning and solution testing includes the following.
- Pre-Intervention literature search and consultation with senior medical, nursing and respiratory clinicians to endorse TSANZ guidelines for Southern NSW Local Health District.
- Endorsed TSANZ guidelines for undertaking spirometry for admitted patient with COPD made available to staff on the intranet.
- Education for medical ward staff on TSANZ guidelines accessible via the intranet and internet.
- Planned regular staff education sessions for spirometry assessment in conjunction with assessing breathlessness with use of Borg Scale and oxygen variance prescription.
- Test understanding and use of TSANZ guidelines for spirometry, breathlessness and oxygen prescription by clinical lead and COPD.
- Provide patient COPD care bundle for personalised goal setting and health literacy.
- Develop draft framework for the proposed COPD support team including governance and Key Performance Indicators.
- Test the COPD Support Team Project objectives through a six week trial in line with the draft framework and ongoing communication plan release.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- March 2018 – Breathe Easy Project Management Plan formalised
- May 2018 – Breathe Easy Diagnostics Report finalised
- July 2018 – Breathe Easy Agreed Solutions Plan completed
- September 2018 – Breathe Easy Solution Implementation Plan formalised with updated communication strategies, risks and issues log, and Gantt chart approvals.
- October 2018 – Breathe Easy project started
- November 2019 – Breathe Easy project planned completion
Implementation sites
Medical ward – South East Regional Hospital, Southern NSW Local Health District, Bega
Partnerships
Centre for Healthcare Redesign
Evaluation
The project evaluation will be ongoing from the start of implementation in October 2018 through to project completion in November 2019. Evaluation includes monitoring, reporting and reviewing the percentage of admitted patients with COPD who have:
- completed spirometry prior to discharge (n=360 p.a.)
- oxygen variance charted (n=360 p.a.)
- completed patient reported outcome measures and patient reported experience measures (n=360 p.a.).7
Lessons learnt
The following aspects were assessed during ward rounding.
Structure
Review the environment in which the healthcare is delivered. Qualitative data showed the two lowest scoring areas for SERH medical ward were:
- organisational stress, which evaluates priorities competing for resources (48.4%)
- involvement, where people were more likely to commit to changes if involved in the planning and implementation (48.2%).
Mitigating barriers identified in survey data
Having strong sponsorship has been a priority to address these challenges and is well recognised as the most important factor in ensuring fast and successful implementation.
Processes
Review the method in which the healthcare is delivered.
Analysis of monitoring data
Cost effectiveness
Ask questions and don’t be afraid of the answers.
Outcomes
Review the consequences of the changes that have been made using quantitative data (check sheets, tally tool computer system, electronic medical record, search and surveys.)
Sustainability
Think outside the square! One key lesson gleaned from the evidence indicates a holistic change is needed to promote and ensure patient safety. This change is developed by learning from failures or barriers and embracing the remarkable successes in a complex system continually striving for improvement. These learnings can be shared locally, nationally, and potentially globally.
References
- Yang IA, Brown JL, George J, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease; 2018. Version 2.54, June 2018. Lung Foundation Australia; 2018.
- Buchan H. Gaps between best evidence and practice: causes for concern. Medical Journal of Australia. 2004;80(Supplement):S48-S9.
- Garling P. Special Commission of Inquiry: Acute Care Services in NSW Public Hospitals. State of NSW; 2008.
- World Health Organization. Realistic medicine to improve the quality of care in Scotland. Geneva: WHO; 2016.
- Kennedy P, Leathley C, Hughes C. Clinical practice variation. Medical Journal of Australia. 2010:193(Supplement 8):S97-S9.
- NSW Agency of Clinical Innovation. Chronic Obstructive Pulmonary Disease Clinical Audit: South East Regional Hospital. Chatswood: ACI; 2017.
- NSW Agency for Clinical Innovation. Patient reported Measures. Chatswood: ACI; 2017.
Further reading
- Aarons G A, Sklar M, Mustanski B, et al. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Science. 2017;12(111).
- Abdo W, Heunks L. Oxygen-induced hypercapnia in COPD: myths and facts. Critical Care. 2012;16(5): 323.
- Christensen C, Bohmer R, Kenagy J. Will Disruptive Innovations Cure Health Care? Harv Bus Rev. 2000 Sep-Oct;78(5):102-12, 199.
- Crabtree B, Nutting P, Miller W, et al. Primary Care Practice Transformation Is Hard Work: Insights from a 15-Year Developmental Program of research. Medical Care. 2011;49(Supplement);S28-S35.
- Denniston A, O'Brien C, Stableforth D. The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre-hospital and hospital emergency management. Clinical Medicine. 2002;2(5): 449-451.
- Freshman B, Rubino L, Chassiakos Y. Collaboration Across the Disciplines in Health Care. Sudbury: Jones and Bartlett Publishers; 2010.
- Haugdahl H, Storli S, Meland B, et al. Underestimation of Patient Breathlessness by Nurses and Physicians during a Spontaneous Breathing Trial. American Journal of Respiratory and Critical Care Medicine. 2015;192(12);1440-1448.
- Porsbjerg C, Sverrild A, Baines K, et al. Advancing the management of obstructive airways diseases through translational research. Clinical & Experimental Allergy - Wiley Online Library. 2018; 48;493-451.
Contact
Christine Sullivan
Nurse Practitioner Chronic and Complex Care
South East Regional Hospital
Southern NSW Local Health District
Phone: 0455 072 922
Christine.Sullivan1@health.nsw.gov.au