This project aims to provide a coordinated, equitable and integrated service for children requiring invasive long term ventilation (LTV), and their families. It also aims to support the needs of LTV children at home and in the community, and provide access to a comprehensive package of ambulatory care services to decrease admission rates and days spent at hospital.
View a poster from the Centre for Healthcare Redesign graduation, December 2018.
Aim
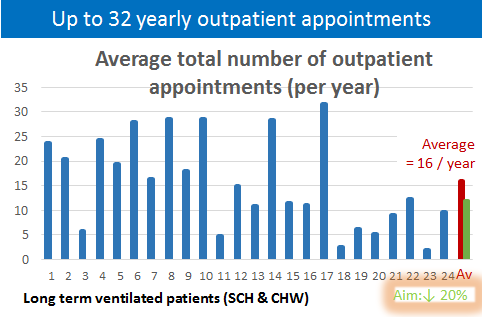
To ensure that all children with LTV needs have an identified coordinating medical lead and awareness of emergency care procedures in the home and community by December 2018. In addition, by July 2019, the number of days that LTV children need to attend outpatient appointments will be reduced by 20%.
Benefits
- A unified governance and operational structure across the Sydney Children’s Hospital Network (SCHN) for LTV patients.
- Clear and consistent eligibility criteria for the LTV service so that children at the highest risk are managed under the governance structures of the service.
- Clear access to ambulatory care supports to minimize Emergency Department presentations and decrease the number of admissions to hospital.
- A consistent approach to the management of children on LTV in the community (including intersection with EnableNSW, National Disability Insurance Agency and local health districts).
- Data and frameworks developed will inform future reviews that may be conducted by the Ministry of Health of the NSW home-based model of care for children on LTV.
- Reduce confusion for patients and their families as well as clinicians who access both hospitals across the Network.
- A strong, coordinated professional voice to advocate for increased support services for LTV patients and their families.
Background
Children who require LTV across SCHN have some of the most complex care needs in the Health system. Currently, SCHN manages 24 children who are ventilated via a tracheostomy, 22 of whom are clinically stable and managed at home.
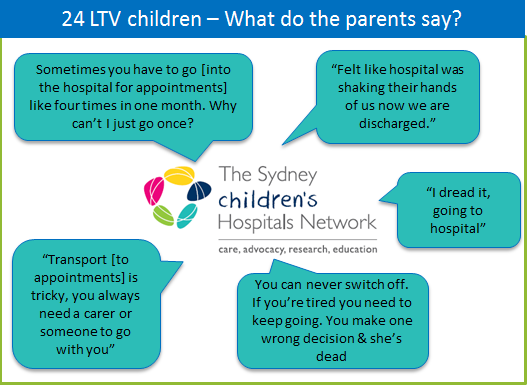
These 24 children have 22 different primary diagnoses and are unified only by their need for long-term invasive ventilation. They will be managed by between 15-20 different clinical teams following discharge and attend as many as 32 outpatient appointments per year (Figure 2). The community management for these children is described as 'frustrating' and 'relentless' by parents who must learn how to navigate fractured health and community systems. Due to their complexity, most LTV children don’t access existing SCHN ambulatory services designed to coordinate care and minimise hospital presentations (e.g. Hospital in the Home and KidsGPS).
It has also been identified across the SCHN that there is poor parent awareness of formal emergency care plans, which are inconsistently updated. Parents and carers report that they felt isolated and overwhelmed after discharge.
A coordinated approach to care for LTV children and their families aims to empower and support families throughout their community journey, minimise risk, build confidence and collaboratively manage care.
We aim to put the child and family at the centre of our practice and determine ways to best support children and reduce the burden of care for families, while maintaining frameworks that ensure quality and safety in the hospital and community.
Implementation
Solution 1 – Implementation of a governance structure for the LTV service
The governance structure for the LTV service has been developed in consultation with clinical and executive leads across the SCHN and EnableNSW. A business case, including a proposed budget for the LTV medical lead and service coordinator positions, has been submitted to the SCHN executive and approved. Positions are currently on the growth funding priority list for 2018-2019. Position descriptions for the LTV medical lead and service coordinator will be reviewed and finalised prior to recruitment.
Solution 2 – Enhance the utilisation of Kids GPS service
KidsGPS is a SCHN-wide service that sits within ambulatory care and aims to assist with the care coordination needs of children with chronic and complex conditions. Prior to this project, LTV children did not access this service. The project team has met with the SCHN manager and staff of KidsGPS and ambulatory care to discuss the development of an LTV pathway of care. This includes delineation of roles and responsibilities of key staff and identifying the training needs of KidsGPS. These aspects will be formalised through the development of an ambulatory model of care for LTV children. Due to the complexity of the cohort, a staggered introduction of the children into KidsGPS is scheduled.
Solution 3 – Development of emergency care plans
Consultation has occurred with the LTV clinical leads to finalise Ambulance NSW Authorised Care Plans. These will be included in individualised care plans that will be completed by KidsGPS. These care plans will form part of the emergency management documentation that will be carried by families and made available on SCHN databases. Consultation continues with key clinical staff in the emergency departments to operationalize emergency management plans across sites.
Solution 4 – More consistent utilisation of Hospital in The Home (HiTH) service
Project staff will continue to meet with the Network manager and staff of ambulatory care services to develop operational guidelines for the use of this service for LTV children.
Solution 5 – Utilising telehealth in outpatient appointments
To minimise the number of times LTV children and their families have to visit the hospital for outpatient appointments, the service is looking to implement telehealth for scheduled outpatient appointments. Further consultation with the digital health coordinator and relevant services will determine how to operationalise telehealth for this cohort.
Status
Implementation – The project is ready for implementation and is currently being implemented and piloted.
Dates
- Start Date: February 2018
- End Date: July 2019
Implementation sites
- Sydney Children’s Hospitals Network
- The Children’s Hospital at Westmead
- Sydney Children’s Hospital, Randwick
Partnerships
- EnableNSW, Healthshare
- Centre for Healthcare Redesign
Evaluation
As of October 2018, the ‘Breath of Fresh Air’ project has prioritised Solutions 1, 2 and 3 for implementation.
Outcomes that will be measured as part of the final evaluation in July 2019 include the following.
Solution 1 – Implementation of a governance structure for the LTV service
SCHN will have an endorsed governance structure for the LTV service and roles and responsibilities (including position descriptions) for a LTV medical lead and coordinator at both sites. Once this is in place, 100% of LTV children will have an identified LTV coordinating medical lead on discharge, from a baseline of 25%.
Solution 2 – Enhance the utilisation of KidsGPS service
Increase KidsGPS use from 0% to 50% by March 2019. To date, we have transitioned 37.5% of LTV children onto KidsGPS and are continuously evaluating and refining the process based on parent and staff feedback.
Solution 3 – Development of emergency care plans
A formal evaluation of patient awareness will be completed by July 2019. Parents have anecdotally reported an increase in communication and clarity between teams.
The number of up-to-date and completed Authorised Care Plans will have improved from 46% to 100% by December 2018. Currently 80% are updated.
Solution 4 – More consistent utilisation of HiTH service
Increase consistent referrals to HiTH services from 0% to 50% by March 2019. We are currently testing the use of the HiTH pathway with one patient/family using a continuous improvement approach.
Solution 5 – Utilising telehealth in outpatient appointments
Implementation of this solution has not commenced. We are partnering with the SCHN integrated care telehealth project to enable the effective and appropriate use of telehealth.
Lessons learnt
This project included the two paediatric hospitals of the SCHN. It involved multiple disciplines, services, departments, processes and governance structures. During stakeholder workshops, it became apparent that each site had unique issues to be considered when designing solutions. Strong sponsorship to ensure both hospital sites have strong face to face representation during diagnostic, solution and implementation design was necessary.
Despite using existing services of the hospital network such as HiTH and KidsGPS, it is apparent that when including a cohort as medically complex as the LTV group, general guidelines and processes from these services do not automatically transfer. It is important to incorporate the complexities and responsibilities of assisting this patient group through the implementation using a co-design framework as well as ongoing coaching and training for staff.
Further reading
- Amin R, MacLusky I, Zielinski D, et al. Pediatric home mechanical ventilation: A Canadian Thoracic Society clinical practice guideline executive summary. Canadian Journal of Respiratory, Critical Care and Sleep Medicine. 2017;1(1):7-36.
Contact
Erin Krisenthal
Case Coordinator Long Term Ventilation / Project Lead
Sydney Children’s Hospitals Network
0437 575 506
Erin.krisenthal@health.nsw.gov.au