For people who have had one osteoporotic fracture, around half will have a secondary fracture in their lifetime. While local specialist services are available to help prevent secondary fracture, in the Richmond area, only 10% of those at risk are being assessed. This project will improve identification and referral for at-risk patients and help improve patient awareness of the risk of secondary fracture.
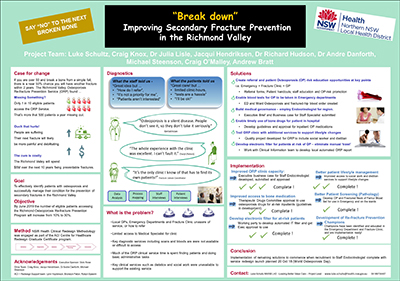
View a poster from the Centre for Healthcare Redesign graduation, August 2018.
Aim
By June 2019 the number of eligible patients accessing the Richmond Osteoporosis Refracture Prevention Program will increase from 10% to 50%.
Benefits
Organisational benefits
- Significant cost savings due to lower incidence of refracturing
- Improved patient satisfaction with healthcare services
- Improved integration of primary health and local health district services
- Opportunity to share the service model with other areas of the health district
Patient benefits
- Prevention of pain and suffering
- Prevention of social and financial impact from injury recovery
- Long-term bone health and protection
- A better healthcare experience
Background
Osteoporosis is a weakening of bones common in women aged over the age of 50. Breaking a bone after a simple fall is often a sign that a person has osteoporosis but around 80% of people who should be tested for osteoporosis when they break a bone are missed. This is a missed opportunity for patient care as there are drugs, and activities such as diet and exercise, that can help strengthen bones and prevent them from refracturing.
The osteoporosis refracture prevention service in the Richmond region of the Northern NSW Local Health District was established in 2015. Despite the quality of care provided, the service has struggled to get patients through the door and only 10% of patients who attend the service complete their program of care.
A number of health service, and patient barriers were identified as contributing to the problem, including poor patient and health provider awareness of the risk.
Implementation
Strategies
- Train emergency department doctors and nurses in the identification of at risk patients, and osteoporosis refracture prevention.
- Train hospital based orthopaedic doctors and staff working in fracture management services (fracture clinic) to identify at risk patients and refer them to osteoporosis refracture prevention service.
- Provide osteoporosis blood sets for doctors working in emergency to enable timely testing for osteoporosis.
- Improve availability of medical officer services to the osteoporosis refracture prevention service through improved governance and use of resources such as telehealth.
- Improve patient referral process to local community health providers to help maintain lifestyle changes for better bone health such as diet, exercise, and smoking cessation.
Status
Pre-implementation – Planning for the project is well underway. Clinician and consumer consultation has occurred but no solutions have been developed.
Dates
October 2017 – June 2019
Implementation sites
Lismore Base Hospital and the Richmond region of the Northern NSW Local Health District
Partnerships
- Agency for Clinical Innovation – Musculoskeletal Network
- Agency for Clinical Innovation – Centre for Healthcare Redesign
- North Coast Primary Health Network
Evaluation
The success of the project will be measured by changes in patient attendance numbers and service recommendations. The data will be available via established databases for the program as recommended under the ACI Model of Care for Osteoporosis Refracture Prevention1. The following measures will be taken each month.
- Number of patients identified and screened for osteoporosis risk.
- Number of patients attending the Richmond osteoporosis refracture prevention service.
- Number of patients commencing an osteoporosis management plan.
- Number of patients remaining on a management plan after six months.
Lessons learnt
- Ensure permission is sought from operational managers before approaching clinical teams.
- The value of face-to-face engagement with primary health providers (e.g. general practitioners).
References
- Agency for Clinical Innovation. Model of Care for Osteoporotic Refracture Prevention. 2nd ed. Chatswood: ACI; 2018.
Further reading
- International Osteoporosis Foundation. Preventing Osteoporosis. Nyon: IOF; 2017.
- Agency for Clinical Innovation. Leading Better Value Care: Osteoporotic Refracture Prevention. Chatswood: ACI; 2018.
Contact
Luke Schultz
Leading Better Value Care - Musculoskeletal Lead
Northern NSW Local Health District
0418974467
Luke.schultz@ncahs.health.nsw.gov.au